primary prevention of coeliac disease - Associazione Italiana ...
primary prevention of coeliac disease - Associazione Italiana ...
primary prevention of coeliac disease - Associazione Italiana ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
MECHANISMS OF ORAL TOLERANCE<br />
65<br />
site <strong>of</strong> gluten exposure, the small intestine.<br />
Experimental models <strong>of</strong> oral tolerance differ from CD in certain respects. In CD, the<br />
most prominent evidence <strong>of</strong> inflammation occurs locally, where antigen exposure takes<br />
place. This is not the case in animals in which the effect <strong>of</strong> abrogation <strong>of</strong> oral tolerance<br />
predominantly affects systemic immune responses. However, in some animal models,<br />
18<br />
oral challenge with the antigen was shown to cause a mild mucosal lesion . Of interest,<br />
there is also evidence that gluten intolerance is associated with systemic damage in<br />
some individuals, as represented by <strong>disease</strong>s such as dermatitis herpetiformis, epilepsy<br />
19-21<br />
and cerebellar ataxia . Moreover, there is some evidence that CD is also associated<br />
with inflammation in the distal intestine and rectal histological changes have been<br />
22<br />
reported . Finally, it is worth noting that systemic antibody responses to gluten are<br />
found in a range <strong>of</strong> disorders, in the absence <strong>of</strong> local gut damage or evidence that these<br />
23<br />
antibodies have a systemic pathogenic significance .<br />
Interest in oral tolerance<br />
Over the decades, an interest in the topic <strong>of</strong> oral tolerance has persisted, in the belief<br />
that its study could lead to a more fundamental understanding <strong>of</strong> homeostasis <strong>of</strong> the<br />
immune system. Furthermore, it is postulated that systemic inflammatory <strong>disease</strong>s<br />
14<br />
might be controlled by inducing oral tolerance to the stimulating antigen . According<br />
to this concept, the administration <strong>of</strong> oral antigen (such as the autoantigenic target <strong>of</strong><br />
systemic <strong>disease</strong>) could lead to a reduced or aborted systemic response to this antigen.<br />
Thus various feeding studies with myelin basic protein (in patients with multiple<br />
24 25<br />
sclerosis ) and collagen (in patients with rheumatoid arthritis ) have been described.<br />
Little therapeutic benefit has been noted in these studies to-date.<br />
Finally, an understanding <strong>of</strong> oral tolerance mechanisms is pertinent to the<br />
development <strong>of</strong> oral vaccines, since this route <strong>of</strong> vaccination is designed to give not<br />
only a local protective immune response, but also systemic protection.<br />
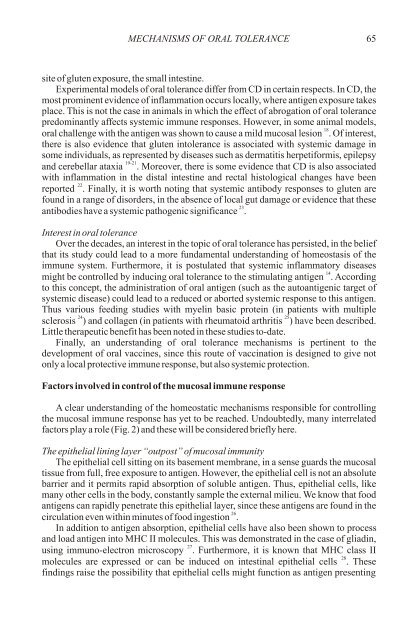
Factors involved in control <strong>of</strong> the mucosal immune response<br />
A clear understanding <strong>of</strong> the homeostatic mechanisms responsible for controlling<br />
the mucosal immune response has yet to be reached. Undoubtedly, many interrelated<br />
factors play a role (Fig. 2) and these will be considered briefly here.<br />
The epithelial lining layer “outpost” <strong>of</strong> mucosal immunity<br />
The epithelial cell sitting on its basement membrane, in a sense guards the mucosal<br />
tissue from full, free exposure to antigen. However, the epithelial cell is not an absolute<br />
barrier and it permits rapid absorption <strong>of</strong> soluble antigen. Thus, epithelial cells, like<br />
many other cells in the body, constantly sample the external milieu. We know that food<br />
antigens can rapidly penetrate this epithelial layer, since these antigens are found in the<br />
26<br />
circulation even within minutes <strong>of</strong> food ingestion .<br />
In addition to antigen absorption, epithelial cells have also been shown to process<br />
and load antigen into MHC II molecules. This was demonstrated in the case <strong>of</strong> gliadin,<br />
27<br />
using immuno-electron microscopy . Furthermore, it is known that MHC class II<br />
28<br />
molecules are expressed or can be induced on intestinal epithelial cells . These<br />
findings raise the possibility that epithelial cells might function as antigen presenting