European Journal of Medical Research - Deutsche AIDS ...
European Journal of Medical Research - Deutsche AIDS ...
European Journal of Medical Research - Deutsche AIDS ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
72 EUROPEAN JOURNAL OF MEDICAL RESEARCH<br />
June 27, 2007<br />
tent, generally well-tolerated, QD protease inhibitor with a<br />
relatively low rate <strong>of</strong> ALT/AST elevations similar to comparators.<br />
Patients with co-infection from 4 ATV clinical development<br />
studies were analyzed.<br />
Methods: This post-hoc analysis <strong>of</strong> studies in ARV-naïve<br />
(BMS 034, 089) and experienced (BMS 043, 045) patients using<br />
ATV, with/without RTV, was performed to assess the rate<br />
<strong>of</strong> ALT, AST, total bilirubin elevations and AEs in the presence<br />
or absence <strong>of</strong> hepatitis co-infection.<br />
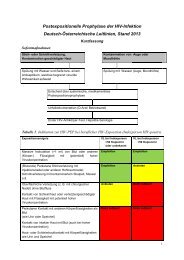
Results: 866 subjects received ATV-based regimens (214<br />
ATV/r; 652 ATV) for a median <strong>of</strong> 48 to 95 weeks (1100 subject-years<br />
<strong>of</strong> treatment exposure). 134 (15%) had baseline<br />
HBV and/or HCV co-infection (Table 1).<br />
Grade 3-4 total bilirubin elevation rates were comparable in<br />
subjects with/without co-infection. Subjects who received<br />
ATV/r or ATV, with/without co-infection, had similar rates <strong>of</strong><br />
Grade 2-4 treatment-related AEs (including jaundice and scleral<br />
icterus) and liver-related AEs.<br />
Conclusions: Similar to other ARVs, patients with HBV<br />
and/or HCV co-infection had a higher rate <strong>of</strong> G3/4 ALT/AST<br />
elevations. In contrast, G3/4 bilirubin elevations, overall AEs<br />
and liver-related AEs, had a comparable frequency in patients<br />
with/without co-infection, suggesting that ATV and ATV/r<br />
are safe treatment alternatives in this population.<br />
C.7 (Poster)<br />
Ocular syphilis prefers different anatomical<br />
structures in HIV–negative and -positive patients<br />
Kunkel J. 1 , Schürmann D. 2 , Kneifel C. 3 , Zeitz M. 1 ,<br />
Pleyer U. 4 , Krause L. 3 , Schneider T. 1<br />
1 Charité Campus Benjamin Franklin, Med. Klinik I,<br />
Gastroenterologie, Infektiologie, Rheumatologie, Berlin,<br />
Germany, 2 Charité Campus Virchow Klinikum, Med. Klinik<br />
m. S. Infektiologie, Berlin, Germany, 3 Charité Campus<br />
Benjamin Franklin, Klinik für Augenheilkunde, Berlin,<br />
Germany, 4 Charité Campus Virchow Klinikum, Klinik für<br />
Augenheilkunde, Berlin, Germany<br />
Objective: To evaluate differences in ocular syphilis between<br />
HIV-negative and –positive patients.<br />
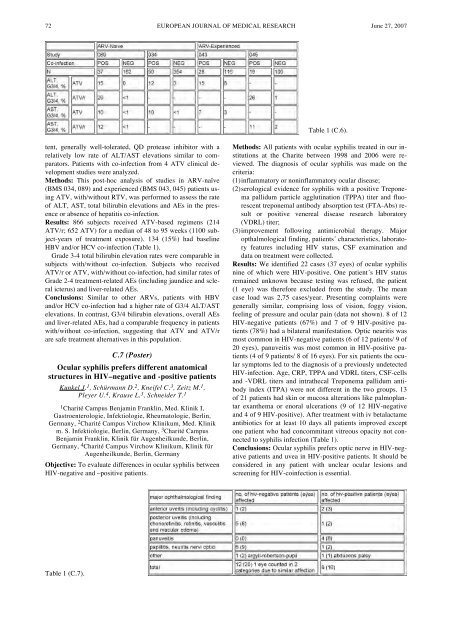
Table 1 (C.7).<br />
Table 1 (C.6).<br />
Methods: All patients with ocular syphilis treated in our institutions<br />
at the Charite between 1998 and 2006 were reviewed.<br />
The diagnosis <strong>of</strong> ocular syphilis was made on the<br />
criteria:<br />
(1)inflammatory or noninflammatory ocular disease;<br />
(2)serological evidence for syphilis with a positive Treponema<br />
pallidum particle agglutination (TPPA) titer and fluorescent<br />
treponemal antibody absorption test (FTA-Abs) result<br />
or positive venereal disease research laboratory<br />
(VDRL) titer;<br />
(3)improvement following antimicrobial therapy. Major<br />
opthalmological finding, patients´ characteristics, laboratory<br />
features including HIV status, CSF examination and<br />
data on treatment were collected.<br />
Results: We identified 22 cases (37 eyes) <strong>of</strong> ocular syphilis<br />
nine <strong>of</strong> which were HIV-positive. One patient´s HIV status<br />
remained unknown because testing was refused, the patient<br />
(1 eye) was therefore excluded from the study. The mean<br />
case load was 2,75 cases/year. Presenting complaints were<br />
generally similar, comprising loss <strong>of</strong> vision, foggy vision,<br />
feeling <strong>of</strong> pressure and ocular pain (data not shown). 8 <strong>of</strong> 12<br />
HIV-negative patients (67%) and 7 <strong>of</strong> 9 HIV-positive patients<br />
(78%) had a bilateral manifestation. Optic neuritis was<br />
most common in HIV-negative patients (6 <strong>of</strong> 12 patients/ 9 <strong>of</strong><br />
20 eyes), panuveitis was most common in HIV-positive patients<br />
(4 <strong>of</strong> 9 patients/ 8 <strong>of</strong> 16 eyes). For six patients the ocular<br />
symptoms led to the diagnosis <strong>of</strong> a previously undetected<br />
HIV-infection. Age, CRP, TPPA and VDRL titers, CSF-cells<br />
and -VDRL titers and intrathecal Treponema pallidum antibody<br />
index (ITPA) were not different in the two groups. 13<br />
<strong>of</strong> 21 patients had skin or mucosa alterations like palmoplantar<br />
exanthema or enoral ulcerations (9 <strong>of</strong> 12 HIV-negative<br />
and 4 <strong>of</strong> 9 HIV-positive). After treatment with iv betalactame<br />
antibiotics for at least 10 days all patients improved except<br />
one patient who had concommitant vitreous opacity not connected<br />
to syphilis infection (Table 1).<br />
Conclusions: Ocular syphilis prefers optic nerve in HIV-negative<br />
patients and uvea in HIV-positive patients. It should be<br />
considered in any patient with unclear ocular lesions and<br />
screening for HIV-coinfection is essential.