Prescription Drug Guide Comprehensive list of covered drugs
Prescription Drug Guide Comprehensive list of covered drugs
Prescription Drug Guide Comprehensive list of covered drugs
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
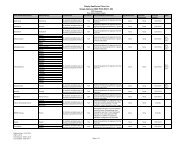
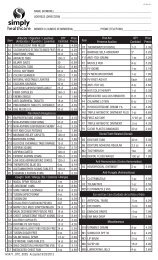
course <strong>of</strong> action for you, we may cover your drug in certain cases during the first 90 days you are amember <strong>of</strong> our plan.For each <strong>of</strong> your <strong>drugs</strong> that is not on our formulary or if your ability to get your <strong>drugs</strong> is limited, we willcover a temporary 30-day supply (unless you have a prescription written for fewer days) when you go toa network pharmacy. After your first 30-day supply, we will not pay for these <strong>drugs</strong>, even if you havebeen a member <strong>of</strong> the plan less than 90 days.If you are a resident <strong>of</strong> a long-term care facility, we will allow you to refill your prescription until wehave provided you with a 93-day transition supply, consistent with the dispensing increment, (unlessyou have a prescription written for fewer days). We will cover more than one refill <strong>of</strong> these <strong>drugs</strong> for thefirst 90 days you are a member <strong>of</strong> our plan. If you need a drug that is not on our formulary or if yourability to get your <strong>drugs</strong> is limited, but you are past the first 90 days <strong>of</strong> membership in our plan, we willcover a 31-day emergency supply <strong>of</strong> that drug (unless you have a prescription for fewer days) while youpursue a formulary exception.For current members who are changing from one treatment setting to another, for example entering along- term care facility from a hospital or being discharged from a hospital to home, the member andprovider will need to utilize our exception and appeals process should the <strong>drugs</strong> not be on our formulary.Members entering or being discharged from a long-term care facility will be allowed a one-timeemergency supply <strong>of</strong> a 31-day supply for medications which the member has not already received atransition supply. In addition, the dispensing pharmacist will need to call the Pharmacy Help Desk toreceive appropriate directions to dispense a prescription required due to a level <strong>of</strong> care change.For more informationFor more detailed information about your Simply Healthcare Plans, Inc. prescription drug coverage,please review your Evidence <strong>of</strong> Coverage and other plan materials.If you have questions about Simply Healthcare Plans, Inc., please call Member Services at 1-877-577-0115. If you use a TTY device, please call 711. We are open 7 days a week, 8 a.m. to 8 p.m. FromFebruary 15 th until September 30 th , you may leave us a voice mail message after hours, Saturdays,Sundays and holidays, and we will return your call the next business day. Or visitwww.mysimplymedicare.com.If you have general questions about Medicare prescription drug coverage, please call Medicare at 1-800-MEDICARE (1-800-633-4227) 24 hours a day/7 days a week. TTY/TDD users should call 1-877-486-2048. Or visit www.medicare.gov.Simply Healthcare Plans, Inc.’s FormularyThe formulary below provides coverage information about some <strong>of</strong> the <strong>drugs</strong> <strong>covered</strong> by SimplyHealthcarePlans, Inc. If you have trouble finding your drug in the <strong>list</strong>, turn to the Index that begins on page 53.The first column <strong>of</strong> the chart <strong>list</strong>s the drug name. Brand name <strong>drugs</strong> are capitalized (e.g., LIPITOR 10MG) and generic <strong>drugs</strong> are <strong>list</strong>ed in lower-case italics (e.g., pravastatin sodium 10 mg).v