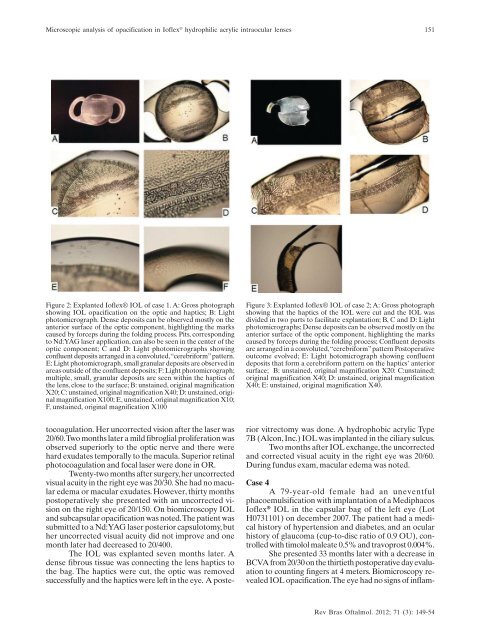
Microscopic analysis of opacification in Ioflex ® hydrophilic acrylic intraocular lenses151Figure 2: Explanted Ioflex® IOL of case 1. A: Gross photographshowing IOL opacification on the optic and haptics; B: Lightphotomicrograph. Dense <strong>de</strong>posits can be observed mostly on theanterior surface of the optic component, highlighting the markscaused by forceps during the folding process. Pits, correspondingto Nd:YAG laser application, can also be seen in the center of theoptic component; C and D: Light photomicrographs showingconfluent <strong>de</strong>posits arranged in a convoluted, “cerebriform” pattern.E: Light photomicrograph, small granular <strong>de</strong>posits are observed inareas outsi<strong>de</strong> of the confluent <strong>de</strong>posits; F: Light photomicrograph;multiple, small, granular <strong>de</strong>posits are seen within the haptics ofthe lens, close to the surface; B: unstained, original magnificationX20; C: unstained, original magnification X40; D: unstained, originalmagnification X100; E, unstained, original magnification X10;F, unstained, original magnification X100Figure 3: Explanted Ioflex® IOL of case 2; A: Gross photographshowing that the haptics of the IOL were cut and the IOL wasdivi<strong>de</strong>d in two parts to facilitate explantation; B, C and D: Lightphotomicrographs; Dense <strong>de</strong>posits can be observed mostly on theanterior surface of the optic component, highlighting the markscaused by forceps during the folding process; Confluent <strong>de</strong>positsare arranged in a convoluted, “cerebriform” pattern Postoperativeoutcome evolved; E: Light hotomicrograph showing confluent<strong>de</strong>posits that form a cerebriform pattern on the haptics’ anteriorsurface; B: unstained, original magnification X20: C:unstained;original magnification X40; D: unstained, original magnificationX40; E: unstained, original magnification X40.tocoagulation. Her uncorrected vision after the laser was20/60. Two months later a mild fibroglial proliferation wasobserved superiorly to the optic nerve and there werehard exudates temporally to the macula. Superior retinalphotocoagulation and focal laser were done in OR.Twenty-two months after surgery, her uncorrectedvisual acuity in the right eye was 20/30. She had no maculare<strong>de</strong>ma or macular exudates. However, thirty monthspostoperatively she presented with an uncorrected visionon the right eye of 20/150. On biomicroscopy IOLand subcapsular opacification was noted. The patient wassubmitted to a Nd:YAG laser posterior capsulotomy, buther uncorrected visual acuity did not improve and onemonth later had <strong>de</strong>creased to 20/400.The IOL was explanted seven months later. A<strong>de</strong>nse fibrous tissue was connecting the lens haptics tothe bag. The haptics were cut, the optic was removedsuccessfully and the haptics were left in the eye. A posteriorvitrectomy was done. A hydrophobic acrylic Type7B (Alcon, Inc.) IOL was implanted in the ciliary sulcus.Two months after IOL exchange, the uncorrectedand corrected visual acuity in the right eye was 20/60.During fundus exam, macular e<strong>de</strong>ma was noted.Case 4A 79-year-old female had an uneventfulphacoemulsification with implantation of a MediphacosIoflex ® IOL in the capsular bag of the left eye (LotH0731101) on <strong>de</strong>cember 2007. The patient had a medicalhistory of hypertension and diabetes, and an ocularhistory of glaucoma (cup-to-disc ratio of 0.9 OU), controlledwith timolol maleate 0.5% and travoprost 0.004%.She presented 33 months later with a <strong>de</strong>crease inBCVA from 20/30 on the thirtieth postoperative day evaluationto counting fingers at 4 meters. Biomicroscopy revealedIOL opacification. The eye had no signs of inflam-Rev Bras Oftalmol. 2012; 71 (3): 149-54
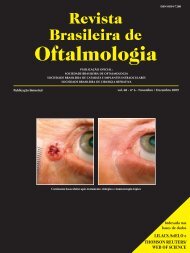
152Ventura BV, Ventura M, Lira W, Ventura CV, Santhiago MR, Werner LFigure 4: Explanted Ioflex ® IOL of case 3; A and B: Lightphotomicrographs showing <strong>de</strong>nse <strong>de</strong>posits mostly on the anteriorsurface of the optic component. Brown <strong>de</strong>posits, consistent withiris pigments, are seen on the lens surface; C: Light photomicrograph.Confluent <strong>de</strong>posits are arranged in a convoluted, “cerebriform”pattern. D: Light photomicrograph showing multiple, small, granular<strong>de</strong>posits within the haptics of the lens, close to the surface.Part of the haptic was cut to facilitate IOL explantation. A:unstained, original magnification X20; B: unstained, originalmagnification X40; C: unstained, original magnification X100; D:unstained, original magnification X100mation. The IOL was explanted 39 months postoperativelyand a hydrophobic acrylic Type 7B (Alcon, Inc.) IOL wasimplanted in the capsular bag. There were no intraoperativeor postoperative complications. The patient’s BCVA1 month after IOL exchange on the left eye was 20/80.Case 5A 78-year-old male was submitted to aphacoemulsification with uneventful implantation of aMediphacos Ioflex ® IOL in the right eye (Lot J0726349)on september 2007 and in the left eye (Lot G0726242)on october 2007. The patient had a medical history ofhypertension and diabetes. There were no intraoperativeor immediate postoperative complications. His fundusexam was normal.He presented 30 months after the surgery in theleft eye with a <strong>de</strong>crease in this eye’s BCVA from 20/20on the thirtieth postoperative day evaluation to 20/150.BCVA in the right eye was preserved. Ocular examinationonly revealed haziness on the left IOL’s surfaces.Vision did not improve after Nd:YAG laser posteriorcapsulotomy. The IOL in the left eye was explanted 41months postoperatively and a PMMA OP-72(Mediphacos, Belo Horizonte, Brazil) IOL was implantedin the sulcus. This eye’s final BCVA was 20/30.Laboratory findingsThe explanted lenses were sent to the IntermountainOcular Research Center (John A. Moran Eye Center,University of Utah, USA) in the dry state. Each lensFigure 5: Light photomicrographs of the explanted Ioflex® incases 1 (A and B) and 4 (C and D). In both cases, the <strong>de</strong>posits weremore concentrated on the anterior surface of the lens and inregions close to the surface. They stained positive for calcium withboth histochemical techniques; A: von Kossa, original magnificationX40; B: von Kossa, original magnification X200; Postoperativeoutcome evolved; C: Alizarin red, original magnification X20; D:Alizarin red, original magnification X100.un<strong>de</strong>rwent gross examination and light microscopy.Gross analyses were performed and photographs weretaken for documentation using a Cyber-shot DSC-F707(Sony, CA, USA). Light microscopy was performed usinga BX40 light microscope (Olympus, Japan) and photomicrographswere taken with a DP20 digital camera(Olympus, Japan) attached to the light microscope.Gross examination of the explanted IOLs showeda whitish discoloration of the specimens. Microscopicexamination showed <strong>de</strong>nse <strong>de</strong>posits forming an almostcontinuous crust, mostly on the anterior surface of theoptic component. Confluent <strong>de</strong>posits were arranged inconvoluted irregular areas forming a “cerebriform” pattern.Small granular <strong>de</strong>posits were observed in areasoutsi<strong>de</strong> of the crust. The <strong>de</strong>posits were most confluentalong linear areas. Multiple, small, granular <strong>de</strong>positswere also generally observed within the optic and hapticsof the lenses, close to the surface. Some peripheral areasof the optic were relatively clear of surface and substance<strong>de</strong>posits/granules (Figures 2, 3 and 4).In case 1, pits, corresponding to Nd:YAG laserapplication, were observed in the optic component. Incase 3, there were brown <strong>de</strong>posits on the lens surfaceconsistent with iris pigments.Selected lenses un<strong>de</strong>rwent further examination.Two sagittal cuts were performed at the optic componentof the lenses in cases 1 and 4 to obtain an optical cylin<strong>de</strong>r.In case 1, the cylin<strong>de</strong>r was processed and multiple sagittalcuts were stained with the von Kossa method for calcium.In case 4, the cylin<strong>de</strong>r and the remain<strong>de</strong>r of the lens wereRev Bras Oftalmol. 2012; 71 (3): 149-54
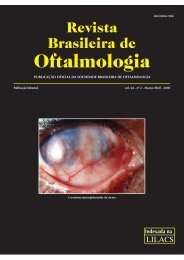
- Page 1 and 2: vol. 71 - nº 3 - Maio/Junho 2012RB
- Page 3 and 4: 144Revista Brasileira de Oftalmolog
- Page 5 and 6: 146173 Características e deficiên
- Page 7 and 8: 148Rezende F, Bisol RAR, Tiago Biso
- Page 9: 150Ventura BV, Ventura M, Lira W, V
- Page 13 and 14: 154Ventura BV, Ventura M, Lira W, V
- Page 15 and 16: 156Moura EM, Volpini M, Moura GAGIN
- Page 17 and 18: 158Moura EM, Volpini M, Moura GAGco
- Page 19 and 20: 160ARTIGO ORIGINALEficácia da comb
- Page 21 and 22: 162Almodin J, Buhler Junior C, Almo
- Page 23 and 24: 164ARTIGO ORIGINALHipermetropia ap
- Page 25 and 26: 166Ambrósio Jr R, Silva RS; Lopes
- Page 27 and 28: 168Ambrósio Jr R, Silva RS; Lopes
- Page 29 and 30: 170Ambrósio Jr R, Silva RS; Lopes
- Page 31 and 32: 172Ambrósio Jr R, Silva RS; Lopes
- Page 33 and 34: 174Ventura CVOC, Gomes MLS, Ventura
- Page 35 and 36: 176Ventura CVOC, Gomes MLS, Ventura
- Page 37 and 38: 178Ventura CVOC, Gomes MLS, Ventura
- Page 39 and 40: 180ARTIGO ORIGINALPeriocular basal
- Page 41 and 42: 182Macedo EMS, Carneiro RC, Carrico
- Page 43 and 44: 184RELATO DE CASODiplopia após inj
- Page 45 and 46: 186Rassi MMO, Santos LHBTABELA 1Per
- Page 47 and 48: 188RELATO DE CASOSíndrome de Down:
- Page 49 and 50: 190Lorena SHTachados de blefarite e
- Page 51 and 52: 192Passos AF, Borges DFINTRODUÇÃO
- Page 53 and 54: 194ARTIGO DE REVISÃOImportance of
- Page 55 and 56: 196Veloso CER, Almeida LNF, De Marc
- Page 57 and 58: 198Veloso CER, Almeida LNF, De Marc
- Page 59 and 60: 200Schellini SA, Sousa RLFINTRODUÇ
- Page 61 and 62:
202Schellini SA, Sousa RLFduzidos m
- Page 63 and 64:
204Schellini SA, Sousa RLF18. Ferra
- Page 65 and 66:
206Instruções aos autoresA Revist
- Page 67:
208RevistaBrasileira deOftalmologia