Final Program - American Society of Gene & Cell Therapy
Final Program - American Society of Gene & Cell Therapy
Final Program - American Society of Gene & Cell Therapy
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
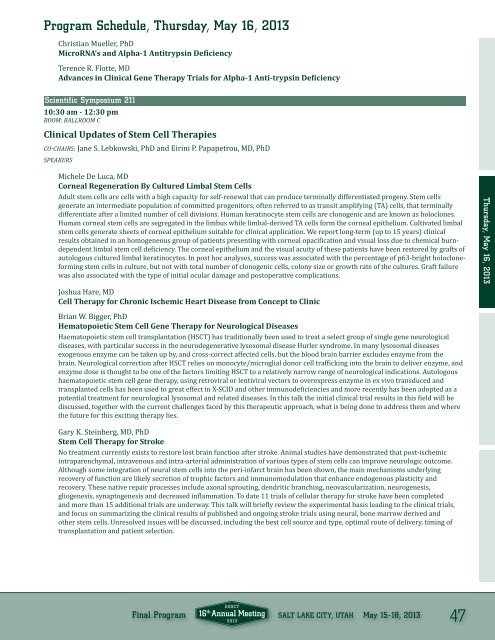
<strong>Program</strong> Schedule, Thursday, May 16, 2013<br />
Christian Mueller, PhD<br />
MicroRNA’s and Alpha-1 Antitrypsin Deiciency<br />
Terence R. Flotte, MD<br />
Advances in Clinical <strong>Gene</strong> <strong>Therapy</strong> Trials for Alpha-1 Anti-trypsin Deiciency<br />
Scientific Symposium 211<br />
10:30 am - 12:30 pm<br />
ROOM: BALLROOM C<br />
Clinical Updates <strong>of</strong> Stem <strong>Cell</strong> Therapies<br />
CO-CHAIRS: Jane S. Lebkowski, PhD and Eirini P. Papapetrou, MD, PhD<br />
SPEAKERS<br />
Michele De Luca, MD<br />
Corneal Regeneration By Cultured Limbal Stem <strong>Cell</strong>s<br />
Adult stem cells are cells with a high capacity for self-renewal that can produce terminally differentiated progeny. Stem cells<br />
generate an intermediate population <strong>of</strong> committed progenitors, <strong>of</strong>ten referred to as transit amplifying (TA) cells, that terminally<br />
differentiate after a limited number <strong>of</strong> cell divisions. Human keratinocyte stem cells are clonogenic and are known as holoclones.<br />
Human corneal stem cells are segregated in the limbus while limbal-derived TA cells form the corneal epithelium. Cultivated limbal<br />
stem cells generate sheets <strong>of</strong> corneal epithelium suitable for clinical application. We report long-term (up to 15 years) clinical<br />
results obtained in an homogeneous group <strong>of</strong> patients presenting with corneal opaciication and visual loss due to chemical burndependent<br />
limbal stem cell deiciency. The corneal epithelium and the visual acuity <strong>of</strong> these patients have been restored by grafts <strong>of</strong><br />
autologous cultured limbal keratinocytes. In post hoc analyses, success was associated with the percentage <strong>of</strong> p63-bright holocloneforming<br />
stem cells in culture, but not with total number <strong>of</strong> clonogenic cells, colony size or growth rate <strong>of</strong> the cultures. Graft failure<br />
was also associated with the type <strong>of</strong> initial ocular damage and postoperative complications.<br />
Joshua Hare, MD<br />
<strong>Cell</strong> <strong>Therapy</strong> for Chronic Ischemic Heart Disease from Concept to Clinic<br />
Thursday, May 16, 2013<br />
Brian W. Bigger, PhD<br />
Hematopoietic Stem <strong>Cell</strong> <strong>Gene</strong> <strong>Therapy</strong> for Neurological Diseases<br />
Haematopoietic stem cell transplantation (HSCT) has traditionally been used to treat a select group <strong>of</strong> single gene neurological<br />
diseases, with particular success in the neurodegenerative lysosomal disease Hurler syndrome. In many lysosomal diseases<br />
exogenous enzyme can be taken up by, and cross-correct affected cells, but the blood brain barrier excludes enzyme from the<br />
brain. Neurological correction after HSCT relies on monocyte/microglial donor cell traficking into the brain to deliver enzyme, and<br />
enzyme dose is thought to be one <strong>of</strong> the factors limiting HSCT to a relatively narrow range <strong>of</strong> neurological indications. Autologous<br />
haematopoietic stem cell gene therapy, using retroviral or lentiviral vectors to overexpress enzyme in ex vivo transduced and<br />
transplanted cells has been used to great effect in X-SCID and other immunodeiciencies and more recently has been adopted as a<br />
potential treatment for neurological lysosomal and related diseases. In this talk the initial clinical trial results in this ield will be<br />
discussed, together with the current challenges faced by this therapeutic approach, what is being done to address them and where<br />
the future for this exciting therapy lies.<br />
Gary K. Steinberg, MD, PhD<br />
Stem <strong>Cell</strong> <strong>Therapy</strong> for Stroke<br />
No treatment currently exists to restore lost brain function after stroke. Animal studies have demonstrated that post-ischemic<br />
intraparenchymal, intravenous and intra-arterial administration <strong>of</strong> various types <strong>of</strong> stem cells can improve neurologic outcome.<br />
Although some integration <strong>of</strong> neural stem cells into the peri-infarct brain has been shown, the main mechanisms underlying<br />
recovery <strong>of</strong> function are likely secretion <strong>of</strong> trophic factors and immunomodulation that enhance endogenous plasticity and<br />
recovery. These native repair processes include axonal sprouting, dendritic branching, neovascularization, neurogenesis,<br />
gliogenesis, synaptogenesis and decreased inlammation. To date 11 trials <strong>of</strong> cellular therapy for stroke have been completed<br />
and more than 15 additional trials are underway. This talk will briely review the experimental basis leading to the clinical trials,<br />
and focus on summarizing the clinical results <strong>of</strong> published and ongoing stroke trials using neural, bone marrow derived and<br />
other stem cells. Unresolved issues will be discussed, including the best cell source and type, optimal route <strong>of</strong> delivery, timing <strong>of</strong><br />
transplantation and patient selection.<br />
<strong>Final</strong> <strong>Program</strong> SALT LAKE CITY, UTAH May 15–18, 2013<br />
47