- Page 1 and 2:
Clinical Practice Guidelinefor Eati
- Page 3:
This clinical practice guideline (C
- Page 6 and 7:
Annex 2.7. Diagnostic Criteria for
- Page 8 and 9:
This CPG aims to provide the popula
- Page 11 and 12:
External Review of Patient Informat
- Page 13 and 14:
14. What is the efficacy and safety
- Page 15 and 16:
CLINICAL PRACTICE GUIDELINE FOR EAT
- Page 17 and 18:
D 6.2. In anorexia nervosa (AN), we
- Page 19 and 20: D 8.6. Primary care centres should
- Page 21 and 22: 9.GM.02. Before initiating artifici
- Page 23 and 24: Binge-Eating DisorderA 9.3.3.1. A s
- Page 25 and 26: D 9.GP.11. In children and adolesce
- Page 27 and 28: Binge-Eating DisorderD 9.GPH.6. In
- Page 29 and 30: 11. Prognosis of Eating Disorders (
- Page 31 and 32: ED: Eating disorderEDNOS: Eating di
- Page 33 and 34: 1. IntroductionBackgroundThe develo
- Page 35 and 36: However, there is a need for a guid
- Page 37 and 38: Table 2. Studies on the prevalence
- Page 39 and 40: 2. Scope and ObjectivesTarget Popul
- Page 41 and 42: Aspects not included in the CPGThe
- Page 43 and 44: 3. MethodologyThe methodology emplo
- Page 45 and 46: - Synthesis and analysis of the sci
- Page 47 and 48: 4. Definition and Classification of
- Page 49 and 50: - Other psychopathological disturba
- Page 51 and 52: Sociocultural factorsThe studies id
- Page 53 and 54: accompany eating disorders. However
- Page 55 and 56: 5. Prevention of Eating DisordersKe
- Page 57 and 58: (causal factors). Participants in t
- Page 59 and 60: is a programme that promotes a heal
- Page 61 and 62: MA 1341++MA 1341++No definitive con
- Page 63 and 64: Of all the proposed criteria and re
- Page 65 and 66: Spanish version of the EAT-40In Spa
- Page 67 and 68: of the five dimension results in th
- Page 69: 6.5. It is recommended to use quest
- Page 73 and 74: to help them cope with the situatio
- Page 75 and 76: Other examinationsTo ascertain whet
- Page 77 and 78: CLINICAL PRACTICE GUIDELINE FOR EAT
- Page 79 and 80: - Initiating nutritional treatment
- Page 81 and 82: 8.2. In eating disorders, what clin
- Page 83 and 84: 8.3.2. Criteria for admission to da
- Page 85 and 86: RecommendationsD 8.1. Individuals w
- Page 87 and 88: 9. Treatment of Eating DisordersThe
- Page 89 and 90: An RCT (Rigaud, 2007; France) 203 c
- Page 91 and 92: 9.2. Nutritional Counselling (NC)9.
- Page 93 and 94: Recommendations(See recommendations
- Page 95 and 96: Anorexia nervosaRecommendationsD 9.
- Page 97 and 98: PSYCHOLOGICAL THERAPIESIn this sect
- Page 99 and 100: Summary of the Evidence(See also th
- Page 101 and 102: There is limited evidence to sugges
- Page 103 and 104: In an RCT (Wilson, 2002; USA) 234 C
- Page 105 and 106: SRSE 2401++SRSE 2401++CBT treatment
- Page 107 and 108: In an RCT (Bulik, 1998) 236 the ove
- Page 109 and 110: Evidence indicates that it is unlik
- Page 111 and 112: A 9.3.3.1. Adult patients with BED
- Page 113 and 114: In an RCT (Carter, 2003; Canada) 24
- Page 115 and 116: Variable: reduction / remission of
- Page 117 and 118: In yet another RCT (Carter, 1998 26
- Page 120 and 121:
Scientific EvidenceThere is insuffi
- Page 122 and 123:
Recommendations(See also recommenda
- Page 124 and 125:
Summary of the Evidence(See summary
- Page 126 and 127:
In an RCT (Lock, 2005) 271 , 20% of
- Page 128 and 129:
Summary of the Evidence(See summary
- Page 130 and 131:
Summary of the Evidence(See summary
- Page 132 and 133:
elaborated by the AHRQ of the US (2
- Page 134 and 135:
SUMMARY OF THE EVIDENCE FORPSYCHOLO
- Page 136 and 137:
D 9.GP.6. For patients with AN who
- Page 138 and 139:
PHARMACOLOGICAL TREATMENTIn this se
- Page 140 and 141:
9.9.1.2. What is the safety of anti
- Page 142 and 143:
There is strong evidence that antid
- Page 144 and 145:
Summary of the EvidenceSRSE 311++SR
- Page 146 and 147:
There is insufficient evidence sugg
- Page 148 and 149:
An RCT (Appolinario, 2003; Brazil)
- Page 150 and 151:
9.10. AntipsychoticsEvidence in AN
- Page 152 and 153:
9.11.2. What is the safety of cypro
- Page 154 and 155:
9.13.1.2. What is the safety of top
- Page 156 and 157:
Recommendations(See recommendations
- Page 158 and 159:
SUMMARY OF THE EVIDENCE FORPHARMACO
- Page 160 and 161:
COMBINED INTERVENTIONSThis section
- Page 162 and 163:
Antidepressants vs. antidepressants
- Page 164 and 165:
There is insufficient evidence to s
- Page 166 and 167:
Summary of the EvidenceSRSE 311++SR
- Page 168 and 169:
9.16.3. Binge-eating disorder9.16.3
- Page 170 and 171:
TREATMENT OF EATING DISORDERS THATO
- Page 172 and 173:
TREATMENT OF CHRONIC EATING DISORDE
- Page 174 and 175:
10. Assessment of Eating DisordersK
- Page 176 and 177:
EDI-2 (Version 2 of the EDI-1)Later
- Page 178 and 179:
BIABody Image Assessment. Collins,
- Page 180 and 181:
10.1.5. The use of questionnaires a
- Page 182 and 183:
has been widely used. It consists o
- Page 184 and 185:
out as the most adequate, given its
- Page 186 and 187:
abuse/dependency, low sensation see
- Page 188 and 189:
the freedom of articles 17 of the S
- Page 190 and 191:
12.2. Is the informed consent of an
- Page 192 and 193:
RecommendationAccording to current
- Page 194 and 195:
CLINICAL PRACTICE GUIDELINE FOR EAT
- Page 196 and 197:
CLINICAL PRACTICE GUIDELINE FOR EAT
- Page 198 and 199:
Algorithm 2. Intervention if there
- Page 200 and 201:
9) Day care admission criteria:- Fr
- Page 202 and 203:
- Oral nutritional support in eatin
- Page 204 and 205:
Algorithm 4. Treatment of BN and BE
- Page 206 and 207:
14.Dissemination and implementation
- Page 208 and 209:
IntegralcareOutcomeSatisfaction ind
- Page 210 and 211:
15. Future research recommendations
- Page 212 and 213:
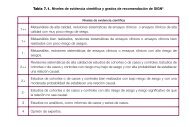
Annex 1. Levels of Evidence and Gra
- Page 214 and 215:
Annex 2. Clinical chaptersAnnex 2.1
- Page 216 and 217:
30. I eat diet food.31. I feel food
- Page 218 and 219:
Annex 2.4. Spanish version of the C
- Page 220 and 221:
6. Do you feel you have control ove
- Page 222 and 223:
20. I feel sad after eating more th
- Page 224 and 225:
33. APPLICABLE ONLY TO WOMEN. My la
- Page 226 and 227:
12. Do you eat reasonable amounts o
- Page 228 and 229:
Annex 2.7. Diagnostic Criteria for
- Page 230 and 231:
Within each guideline some variatio
- Page 232 and 233:
Bulimia nervosa (307.51)Diagnostic
- Page 234 and 235:
Annex 2.8. Spanish version of the E
- Page 236 and 237:
Formula:Patients with eating disord
- Page 238 and 239:
Annex 3. Information for patients w
- Page 240 and 241:
Alert SignsWhat signs can alert us
- Page 242 and 243:
members can seek support and guidan
- Page 244 and 245:
therapist who guides the sessions a
- Page 246 and 247:
negative attitudes towards weight a
- Page 248 and 249:
PizotifenThis drug belongs to the g
- Page 250 and 251:
TopiramateAnticonvulsant psychoacti
- Page 252 and 253:
BULIT Bulimia TestBULIT-R Revised v
- Page 254 and 255:
ISCIII Carlos III Health InstituteI
- Page 256 and 257:
CLINICAL PRACTICE GUIDELINE FOR EAT
- Page 258 and 259:
General Directorate for Public Heal
- Page 260 and 261:
2) We identified 20 documents elabo
- Page 262 and 263:
estimator, establishing the followi
- Page 264 and 265:
CLINICAL PRACTICE GUIDELINE FOR EAT
- Page 266 and 267:
17. Detecció i orientacions terap
- Page 268 and 269:
59. Lo importante es tu vida. No la
- Page 270 and 271:
98. Garner DM. Pathogenesis of anor
- Page 272 and 273:
141. Wilksch SM, Tiggemann M, Wade
- Page 274 and 275:
181. Rivas T, Jiménez M, Bersabé
- Page 276 and 277:
224. Fairburn CG, Jones R, Peveler
- Page 278 and 279:
262. McCann UD, Agras WS. Successfu
- Page 280 and 281:
302. McElroy SL, Casuto LS, Nelson
- Page 282 and 283:
341. Hodes M, Timimi S, Robinson P.
- Page 284 and 285:
388. Steinhausen HC. The outcome of
- Page 286 and 287:
427. Finnish Medical Society Duodec