Strabismus - Fundamentals of Clinical Ophthalmology.pdf
Strabismus - Fundamentals of Clinical Ophthalmology.pdf
Strabismus - Fundamentals of Clinical Ophthalmology.pdf
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
STRABISMUS<br />
Iatrogenic deprivation amblyopia<br />
The treatment <strong>of</strong> an ocular condition such as<br />
an eyelid lesion or corneal ulcer with an<br />
occluding eye patch may also result in<br />
deprivation amblyopia, especially in the first<br />
weeks <strong>of</strong> life. Occlusion may be safe if not used<br />
for more than 80% <strong>of</strong> the waking day. In a<br />
unilateral dense cataract at birth or bilateral<br />
dense cataract at birth requiring surgery,<br />
bilateral occlusion in the early weeks <strong>of</strong> life may<br />
prolong the critical period. This allows more<br />
time to achieve equal imaging in both eyes and<br />
reduce the risk <strong>of</strong> amblyopia.<br />
“Concomitant” strabismus<br />
Congenital esotropia syndromes<br />
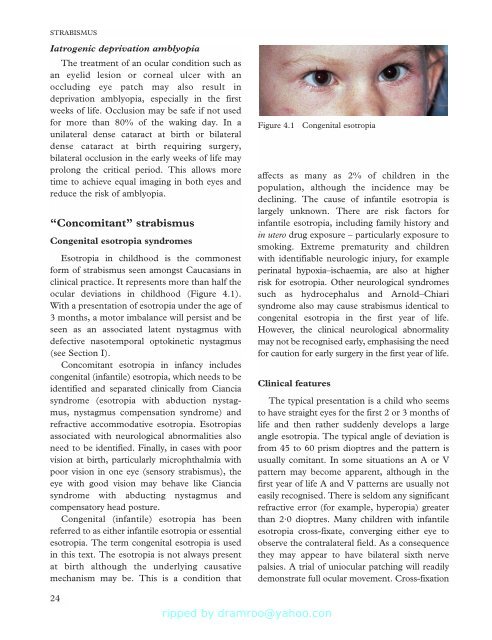
Esotropia in childhood is the commonest<br />
form <strong>of</strong> strabismus seen amongst Caucasians in<br />
clinical practice. It represents more than half the<br />
ocular deviations in childhood (Figure 4.1).<br />
With a presentation <strong>of</strong> esotropia under the age <strong>of</strong><br />
3 months, a motor imbalance will persist and be<br />
seen as an associated latent nystagmus with<br />
defective nasotemporal optokinetic nystagmus<br />
(see Section I).<br />
Concomitant esotropia in infancy includes<br />
congenital (infantile) esotropia, which needs to be<br />
identified and separated clinically from Ciancia<br />
syndrome (esotropia with abduction nystagmus,<br />
nystagmus compensation syndrome) and<br />
refractive accommodative esotropia. Esotropias<br />
associated with neurological abnormalities also<br />
need to be identified. Finally, in cases with poor<br />
vision at birth, particularly microphthalmia with<br />
poor vision in one eye (sensory strabismus), the<br />
eye with good vision may behave like Ciancia<br />
syndrome with abducting nystagmus and<br />
compensatory head posture.<br />
Congenital (infantile) esotropia has been<br />
referred to as either infantile esotropia or essential<br />
esotropia. The term congenital esotropia is used<br />
in this text. The esotropia is not always present<br />
at birth although the underlying causative<br />
mechanism may be. This is a condition that<br />
Figure 4.1<br />
affects as many as 2% <strong>of</strong> children in the<br />
population, although the incidence may be<br />
declining. The cause <strong>of</strong> infantile esotropia is<br />
largely unknown. There are risk factors for<br />
infantile esotropia, including family history and<br />
in utero drug exposure – particularly exposure to<br />
smoking. Extreme prematurity and children<br />
with identifiable neurologic injury, for example<br />
perinatal hypoxia–ischaemia, are also at higher<br />
risk for esotropia. Other neurological syndromes<br />
such as hydrocephalus and Arnold–Chiari<br />
syndrome also may cause strabismus identical to<br />
congenital esotropia in the first year <strong>of</strong> life.<br />
However, the clinical neurological abnormality<br />
may not be recognised early, emphasising the need<br />
for caution for early surgery in the first year <strong>of</strong> life.<br />
<strong>Clinical</strong> features<br />
Congenital esotropia<br />
The typical presentation is a child who seems<br />
to have straight eyes for the first 2 or 3 months <strong>of</strong><br />
life and then rather suddenly develops a large<br />
angle esotropia. The typical angle <strong>of</strong> deviation is<br />
from 45 to 60 prism dioptres and the pattern is<br />
usually comitant. In some situations an A or V<br />
pattern may become apparent, although in the<br />
first year <strong>of</strong> life A and V patterns are usually not<br />
easily recognised. There is seldom any significant<br />
refractive error (for example, hyperopia) greater<br />
than 2·0 dioptres. Many children with infantile<br />
esotropia cross-fixate, converging either eye to<br />
observe the contralateral field. As a consequence<br />
they may appear to have bilateral sixth nerve<br />
palsies. A trial <strong>of</strong> uniocular patching will readily<br />
demonstrate full ocular movement. Cross-fixation<br />
24









![SISTEM SENSORY [Compatibility Mode].pdf](https://img.yumpu.com/20667975/1/190x245/sistem-sensory-compatibility-modepdf.jpg?quality=85)





