Kompendium 2020 Forschung & Klinik
Das Kompendium 2020 der Universitätsklinik für Orthopädie und Unfallchirurgie von MedUni Wien und AKH Wien (o. Univ.-Prof. R. Windhager) stellt einen umfassenden Überblick über die medizinsichen Leistungen und auch die umfangreichen Forschungsfelder dar. Die Veröffentlichungen zeigen die klinische Relevanz und innovative Ansätze der einzelnen Forschungsrichtungen. Herausgeber: Universitätsklinik für Orthopädie und Unfallchirurgie MedUni Wien und AKH Wien Prof. Dr. R. Windhager ISBN 978-3-200-07715-7
Das Kompendium 2020 der Universitätsklinik für Orthopädie und Unfallchirurgie von MedUni Wien und AKH Wien (o. Univ.-Prof. R. Windhager) stellt einen umfassenden Überblick über die medizinsichen Leistungen und auch die umfangreichen Forschungsfelder dar. Die Veröffentlichungen zeigen die klinische Relevanz und innovative Ansätze der einzelnen Forschungsrichtungen.
Herausgeber: Universitätsklinik für Orthopädie und Unfallchirurgie
MedUni Wien und AKH Wien
Prof. Dr. R. Windhager
ISBN 978-3-200-07715-7
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
TOP-Studien<br />
53<br />
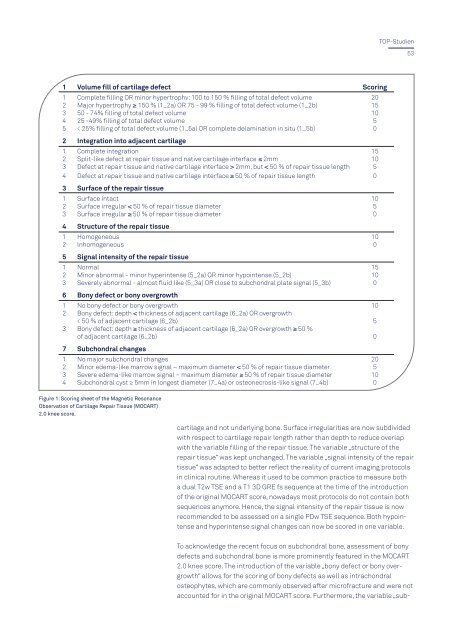
1 Volume fill of cartilage defect Scoring<br />
1 Complete filling OR minor hypertrophv: 100 to 150 % filling of total defect volume 20<br />
2 Major hypertrophy ≥ 150 % (1_2a) OR 75 - 99 % filling of total defect volume (1_2b) 15<br />
3 50 - 74% filling of total defect volume 10<br />
4 25 -49% filling of total defect volume 5<br />
5 < 25% filling of total defect volume (1_5a) OR complete delamination in situ (1_5b) 0<br />
2 Integration into adjacent cartilage<br />
1 Complete integration 15<br />
2 Split-like defect at repair tissue and native cartilage interface ≤ 2mm 10<br />
3 Defect at repair tissue and native cartilage interface > 2mm, but < 50 % of repair tissue length 5<br />
4 Defect at repair tissue and native cartilage interface ≥ 50 % of repair tissue length 0<br />
3 Surface of the repair tissue<br />
1 Surface intact 10<br />
2 Surface irregular < 50 % of repair tissue diameter 5<br />
3 Surface irregular ≥ 50 % of repair tissue diameter 0<br />
4 Structure of the repair tissue<br />
1 Homogeneous 10<br />
2 lnhomogeneous 0<br />
5 Signal intensity of the repair tissue<br />
1 Normal 15<br />
2 Minor abnormal - minor hyperintense (5_2a) OR minor hypointense (5_2b) 10<br />
3 Severely abnormal - almost fluid like (5_3a) OR close to subchondral plate signal (5_3b) 0<br />
6 Bony defect or bony overgrowth<br />
1 No bony defect or bony overgrowth 10<br />
2 Bony defect: depth < thickness of adjacent cartilage (6_2a) OR overgrowth<br />
< 50 % of adjacent cartilage (6_2b) 5<br />
3 Bony defect: depth ≥ thickness of adjacent cartilage (6_2a) OR overgrowth ≥ 50 %<br />
of adjacent cartilage (6_2b) 0<br />
7 Subchondral changes<br />
1 No major subchondral changes 20<br />
2 Minor edema-like marrow signal – maximum diameter < 50 % of repair tissue diameter 5<br />
3 Severe edema-like marrow signal – maximum diameter ≥ 50 % of repair tissue diameter 10<br />
4 Subchondral cyst ≥ 5mm in longest diameter (7_4a) or osteonecrosis-like signal (7_4b) 0<br />
Figure 1: Scoring sheet of the Magnetic Resonance<br />
Observation of Cartilage Repair Tissue (MOCART)<br />
2.0 knee score.<br />
cartilage and not underlying bone. Surface irregularities are now subdivided<br />
with respect to cartilage repair length rather than depth to reduce overlap<br />
with the variable filling of the repair tissue. The variable „structure of the<br />
repair tissue“ was kept unchanged. The variable „signal intensity of the repair<br />
tissue“ was adapted to better reflect the reality of current imaging protocols<br />
in clinical routine. Whereas it used to be common practice to measure both<br />
a dual T2w TSE and a T1 3D GRE fs sequence at the time of the introduction<br />
of the original MOCART score, nowadays most protocols do not contain both<br />
sequences anymore. Hence, the signal intensity of the repair tissue is now<br />
recommended to be assessed on a single PDw TSE sequence. Both hypointense<br />
and hyperintense signal changes can now be scored in one variable.<br />
To acknowledge the recent focus on subchondral bone, assessment of bony<br />
defects and subchondral bone is more prominently featured in the MOCART<br />
2.0 knee score. The introduction of the variable „bony defect or bony overgrowth“<br />
allows for the scoring of bony defects as well as intrachondral<br />
osteophytes, which are commonly observed after microfracture and were not<br />
accounted for in the original MOCART score. Furthermore, the variable „sub-