A Textbook of Clinical Pharmacology and Therapeutics
A Textbook of Clinical Pharmacology and Therapeutics
A Textbook of Clinical Pharmacology and Therapeutics
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
260 ALIMENTARY SYSTEM AND LIVER<br />
LIVER DISEASE<br />
PRINCIPLES UNDERLYING DRUG TREATMENT OF<br />
HEPATIC ENCEPHALOPATHY AND LIVER FAILURE<br />
In severe liver dysfunction, neuropsychiatric changes occur<br />
<strong>and</strong> can progress to coma. The mechanism which produces<br />
these changes is not established, but it is known that in hepatic<br />
coma <strong>and</strong> pre-coma, the blood ammonia concentration<br />
increases. In many patients, the time-course <strong>of</strong> encephalopathy<br />
parallels the rise in blood ammonia concentrations. Orally<br />
administered nitrogenous compounds (e.g. protein, amino<br />
acids, ammonium chloride) yield ammonia in the gut, raise<br />
blood ammonia concentrations <strong>and</strong> provoke encephalopathy.<br />
The liver is the only organ that extracts ammonia from the<br />
blood <strong>and</strong> converts it to urea. Bacterial degradation products<br />
<strong>of</strong> nitrogenous material within the gut enter the systemic circulation<br />
because <strong>of</strong> a failure <strong>of</strong> first-pass hepatic extraction<br />
(due to hepatocellular damage), or due to bypass <strong>of</strong> the hepatocytes<br />
by collateral circulation or intrahepatic shunting.<br />
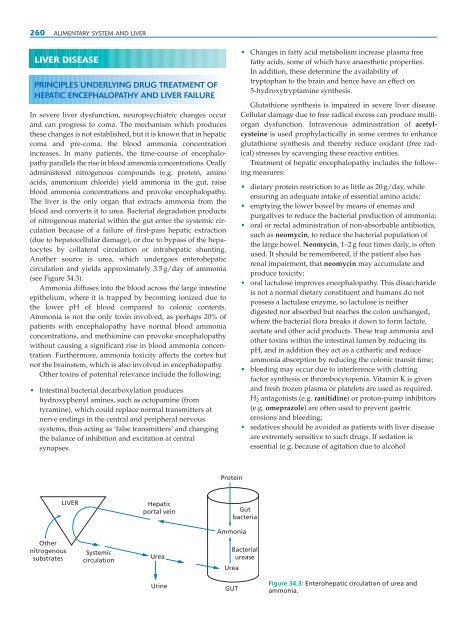
Another source is urea, which undergoes enterohepatic<br />
circulation <strong>and</strong> yields approximately 3.5 g/day <strong>of</strong> ammonia<br />
(see Figure 34.3).<br />
Ammonia diffuses into the blood across the large intestine<br />
epithelium, where it is trapped by becoming ionized due to<br />
the lower pH <strong>of</strong> blood compared to colonic contents.<br />
Ammonia is not the only toxin involved, as perhaps 20% <strong>of</strong><br />
patients with encephalopathy have normal blood ammonia<br />
concentrations, <strong>and</strong> methionine can provoke encephalopathy<br />
without causing a significant rise in blood ammonia concentration.<br />
Furthermore, ammonia toxicity affects the cortex but<br />
not the brainstem, which is also involved in encephalopathy.<br />
Other toxins <strong>of</strong> potential relevance include the following:<br />
• Intestinal bacterial decarboxylation produces<br />
hydroxyphenyl amines, such as octopamine (from<br />
tyramine), which could replace normal transmitters at<br />
nerve endings in the central <strong>and</strong> peripheral nervous<br />
systems, thus acting as ‘false transmitters’ <strong>and</strong> changing<br />
the balance <strong>of</strong> inhibition <strong>and</strong> excitation at central<br />
synapses.<br />
Other<br />
nitrogenous<br />
substrates<br />
LIVER<br />
Systemic<br />
circulation<br />
Hepatic<br />
portal vein<br />
Urea<br />
Urine<br />
Protein<br />
Ammonia<br />
• Changes in fatty acid metabolism increase plasma free<br />
fatty acids, some <strong>of</strong> which have anaesthetic properties.<br />
In addition, these determine the availability <strong>of</strong><br />
tryptophan to the brain <strong>and</strong> hence have an effect on<br />
5-hydroxytryptamine synthesis.<br />
Glutathione synthesis is impaired in severe liver disease.<br />
Cellular damage due to free radical excess can produce multiorgan<br />
dysfunction. Intravenous administration <strong>of</strong> acetylcysteine<br />
is used prophylactically in some centres to enhance<br />
glutathione synthesis <strong>and</strong> thereby reduce oxidant (free radical)<br />
stresses by scavenging these reactive entities.<br />
Treatment <strong>of</strong> hepatic encephalopathy includes the following<br />
measures:<br />
• dietary protein restriction to as little as 20 g/day, while<br />
ensuring an adequate intake <strong>of</strong> essential amino acids;<br />
• emptying the lower bowel by means <strong>of</strong> enemas <strong>and</strong><br />
purgatives to reduce the bacterial production <strong>of</strong> ammonia;<br />
• oral or rectal administration <strong>of</strong> non-absorbable antibiotics,<br />
such as neomycin, to reduce the bacterial population <strong>of</strong><br />
the large bowel. Neomycin, 1–2 g four times daily, is <strong>of</strong>ten<br />
used. It should be remembered, if the patient also has<br />
renal impairment, that neomycin may accumulate <strong>and</strong><br />
produce toxicity;<br />
• oral lactulose improves encephalopathy. This disaccharide<br />
is not a normal dietary constituent <strong>and</strong> humans do not<br />
possess a lactulase enzyme, so lactulose is neither<br />
digested nor absorbed but reaches the colon unchanged,<br />
where the bacterial flora breaks it down to form lactate,<br />
acetate <strong>and</strong> other acid products. These trap ammonia <strong>and</strong><br />
other toxins within the intestinal lumen by reducing its<br />
pH, <strong>and</strong> in addition they act as a cathartic <strong>and</strong> reduce<br />
ammonia absorption by reducing the colonic transit time;<br />
• bleeding may occur due to interference with clotting<br />
factor synthesis or thrombocytopenia. Vitamin K is given<br />
<strong>and</strong> fresh frozen plasma or platelets are used as required.<br />
H 2 antagonists (e.g. ranitidine) or proton-pump inhibitors<br />
(e.g. omeprazole) are <strong>of</strong>ten used to prevent gastric<br />
erosions <strong>and</strong> bleeding;<br />
• sedatives should be avoided as patients with liver disease<br />
are extremely sensitive to such drugs. If sedation is<br />
essential (e.g. because <strong>of</strong> agitation due to alcohol<br />
Gut<br />
bacteria<br />
Bacterial<br />
urease<br />
Urea<br />
GUT<br />
Figure 34.3: Enterohepatic circulation <strong>of</strong> urea <strong>and</strong><br />
ammonia.