A Textbook of Clinical Pharmacology and Therapeutics
A Textbook of Clinical Pharmacology and Therapeutics
A Textbook of Clinical Pharmacology and Therapeutics
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
deficiency. Potassium iodide (3 mg daily p.o.) prevents further<br />
enlargement <strong>of</strong> the gl<strong>and</strong>, but seldom actually shrinks it.<br />
Iodized salt is used to prevent this type <strong>of</strong> endemic goitre in<br />
areas where the diet is iodine deficient, according to a defined<br />
World Health Organization (WHO) policy.<br />
Preoperative treatment with Lugol’s iodine solution (an<br />
aqueous solution <strong>of</strong> iodine <strong>and</strong> potassium iodide) in combination<br />
with carbimazole or propylthiouracil (see below) is<br />
used to reduce the vascularity <strong>of</strong> the gl<strong>and</strong> <strong>and</strong> inhibit thyroid<br />
hormone release. This action <strong>of</strong> iodine in inhibiting thyroid<br />
hormone release is only maintained for one to two weeks,<br />
after which thyroid hormone release is markedly increased if<br />
the cause <strong>of</strong> the hyperthyroidism has not been dealt with.<br />
THYROXINE AND TRI-IODOTHYRONINE<br />
Use<br />
L-Thyroxine is used in the treatment <strong>of</strong> uncomplicated hypothyroidism,<br />
the dose being individualized according to serum<br />
TSH. The dose is titrated every four weeks until the patient has<br />
responded clinically <strong>and</strong> the TSH level has fallen to within the<br />
normal range. Excessive dosage may precipitate cardiac complications,<br />
particularly in patients with ischaemic heart disease in<br />
whom the starting dose should be reduced. If angina pectoris<br />
limits the dose <strong>of</strong> thyroxine, the addition <strong>of</strong> a beta-blocker (e.g.<br />
atenolol) will allow further increments in thyroxine dosage.<br />
Long-term overdosage is undesirable <strong>and</strong> causes osteoporosis,<br />
as well as predisposing to cardiac dysrhythmias.<br />
Congenital hypothyroidism is treated similarly <strong>and</strong> thyroxine<br />
must be given as early as possible. In the UK, the adoption<br />
<strong>of</strong> the Guthrie test has greatly facilitated the early detection <strong>of</strong><br />
neonatal hypothyroidism.<br />
The rapid action <strong>of</strong> T3 is useful in treating myxoedema coma.<br />
It is given intramuscularly while starting maintenance therapy<br />
with thyroxine. Hypothyroidism sometimes coexists with Addison’s<br />
disease (also autoimmune in aetiology) <strong>and</strong> hydrocortisone<br />
is given empirically to patients with myxoedema coma.<br />
Hypothyroidism may result from hypopituitarism. This is<br />
also treated with oral thyroxine in the usual doses. Glucocorticosteroid<br />
replacement must be started first, otherwise<br />
acute adrenal insufficiency will be precipitated.<br />
Mechanism <strong>of</strong> action<br />
Thyroxine is a prohormone. After entering cells it is converted<br />
to T3, which binds to the thyroid hormone nuclear receptor<br />
<strong>and</strong> the lig<strong>and</strong>–receptor complex increases transcription <strong>of</strong><br />
genes involved in the following cellular functions:<br />
• stimulation <strong>of</strong> metabolism – raised basal metabolic rate;<br />
• promotion <strong>of</strong> normal growth <strong>and</strong> maturation, particularly<br />
<strong>of</strong> the central nervous system <strong>and</strong> skeleton;<br />
• sensitization to the effects <strong>of</strong> catecholamines.<br />
Adverse effects<br />
The adverse effects <strong>of</strong> the thyroid hormones relate to their<br />
physiological functions <strong>and</strong> include cardiac dysrhythmia,<br />
angina, myocardial infarction <strong>and</strong> congestive cardiac failure.<br />
ANTITHYROID DRUGS 293<br />
Tremor, restlessness, heat intolerance, diarrhoea <strong>and</strong> other features<br />
<strong>of</strong> hyperthyroidism are dose-dependent toxic effects <strong>of</strong><br />
these hormones. Chronic thyroxine excess is an insidious<br />
cause <strong>of</strong> osteoporosis.<br />
Pharmacokinetics<br />
Thyroid hormones are absorbed from the gut. The effects <strong>of</strong> T4 are not usually detectable before 24 hours <strong>and</strong> maximum<br />
activity is not attained for many days during regular daily<br />
dosing. T3 produces effects within six hours <strong>and</strong> peak activity<br />
is reached within 24 hours. The t1/2 <strong>of</strong> T4 is six to seven days in<br />
euthyroid individuals, but may be much longer than this in<br />
hypothyroidism, <strong>and</strong> that for T3 is two days or less. It is unnecessary<br />
to administer thyroid hormone more frequently than<br />
once a day. The liver conjugates thyroid hormones, which<br />
undergo enterohepatic recirculation.<br />
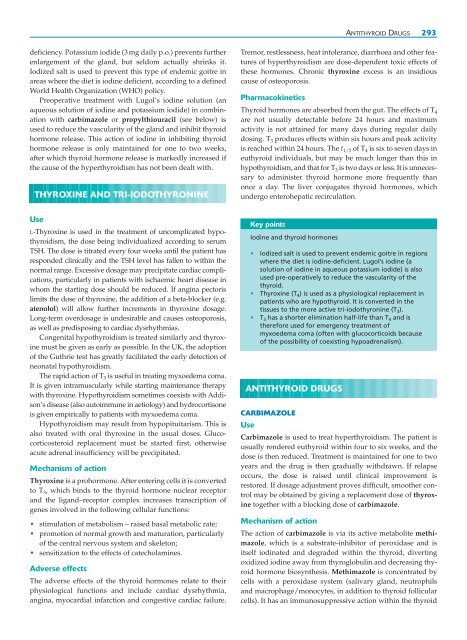
Key points<br />
Iodine <strong>and</strong> thyroid hormones<br />
• Iodized salt is used to prevent endemic goitre in regions<br />
where the diet is iodine-deficient. Lugol’s iodine (a<br />
solution <strong>of</strong> iodine in aqueous potassium iodide) is also<br />
used pre-operatively to reduce the vascularity <strong>of</strong> the<br />
thyroid.<br />
• Thyroxine (T 4) is used as a physiological replacement in<br />
patients who are hypothyroid. It is converted in the<br />
tissues to the more active tri-iodothyronine (T 3).<br />
• T 3 has a shorter elimination half-life than T 4 <strong>and</strong> is<br />
therefore used for emergency treatment <strong>of</strong><br />
myxoedema coma (<strong>of</strong>ten with glucocorticoids because<br />
<strong>of</strong> the possibility <strong>of</strong> coexisting hypoadrenalism).<br />
ANTITHYROID DRUGS<br />
CARBIMAZOLE<br />
Use<br />
Carbimazole is used to treat hyperthyroidism. The patient is<br />
usually rendered euthyroid within four to six weeks, <strong>and</strong> the<br />
dose is then reduced. Treatment is maintained for one to two<br />
years <strong>and</strong> the drug is then gradually withdrawn. If relapse<br />
occurs, the dose is raised until clinical improvement is<br />
restored. If dosage adjustment proves difficult, smoother control<br />
may be obtained by giving a replacement dose <strong>of</strong> thyroxine<br />
together with a blocking dose <strong>of</strong> carbimazole.<br />
Mechanism <strong>of</strong> action<br />
The action <strong>of</strong> carbimazole is via its active metabolite methimazole,<br />
which is a substrate-inhibitor <strong>of</strong> peroxidase <strong>and</strong> is<br />
itself iodinated <strong>and</strong> degraded within the thyroid, diverting<br />
oxidized iodine away from thyroglobulin <strong>and</strong> decreasing thyroid<br />
hormone biosynthesis. Methimazole is concentrated by<br />
cells with a peroxidase system (salivary gl<strong>and</strong>, neutrophils<br />
<strong>and</strong> macrophage/monocytes, in addition to thyroid follicular<br />
cells). It has an immunosuppressive action within the thyroid