A Textbook of Clinical Pharmacology and Therapeutics
A Textbook of Clinical Pharmacology and Therapeutics
A Textbook of Clinical Pharmacology and Therapeutics
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
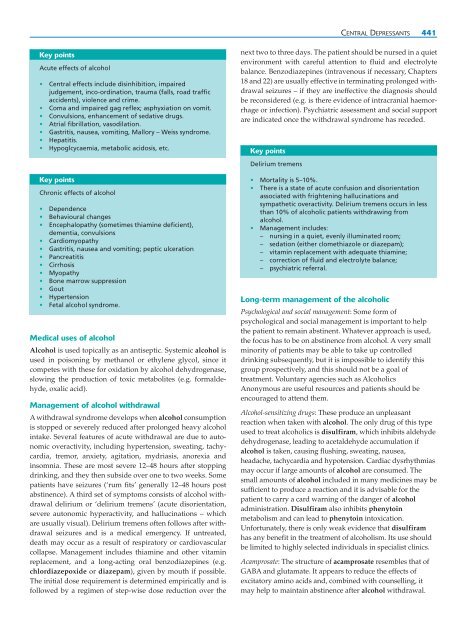
Key points<br />
Acute effects <strong>of</strong> alcohol<br />
• Central effects include disinhibition, impaired<br />
judgement, inco-ordination, trauma (falls, road traffic<br />
accidents), violence <strong>and</strong> crime.<br />
• Coma <strong>and</strong> impaired gag reflex; asphyxiation on vomit.<br />
• Convulsions, enhancement <strong>of</strong> sedative drugs.<br />
• Atrial fibrillation, vasodilation.<br />
• Gastritis, nausea, vomiting, Mallory – Weiss syndrome.<br />
• Hepatitis.<br />
• Hypoglcycaemia, metabolic acidosis, etc.<br />
Key points<br />
Chronic effects <strong>of</strong> alcohol<br />
• Dependence<br />
• Behavioural changes<br />
• Encephalopathy (sometimes thiamine deficient),<br />
dementia, convulsions<br />
• Cardiomyopathy<br />
• Gastritis, nausea <strong>and</strong> vomiting; peptic ulceration<br />
• Pancreatitis<br />
• Cirrhosis<br />
• Myopathy<br />
• Bone marrow suppression<br />
• Gout<br />
• Hypertension<br />
• Fetal alcohol syndrome.<br />
Medical uses <strong>of</strong> alcohol<br />
Alcohol is used topically as an antiseptic. Systemic alcohol is<br />
used in poisoning by methanol or ethylene glycol, since it<br />
competes with these for oxidation by alcohol dehydrogenase,<br />
slowing the production <strong>of</strong> toxic metabolites (e.g. formaldehyde,<br />
oxalic acid).<br />
Management <strong>of</strong> alcohol withdrawal<br />
A withdrawal syndrome develops when alcohol consumption<br />
is stopped or severely reduced after prolonged heavy alcohol<br />
intake. Several features <strong>of</strong> acute withdrawal are due to autonomic<br />
overactivity, including hypertension, sweating, tachycardia,<br />
tremor, anxiety, agitation, mydriasis, anorexia <strong>and</strong><br />
insomnia. These are most severe 12–48 hours after stopping<br />
drinking, <strong>and</strong> they then subside over one to two weeks. Some<br />
patients have seizures (‘rum fits’ generally 12–48 hours post<br />
abstinence). A third set <strong>of</strong> symptoms consists <strong>of</strong> alcohol withdrawal<br />
delirium or ‘delirium tremens’ (acute disorientation,<br />
severe autonomic hyperactivity, <strong>and</strong> hallucinations – which<br />
are usually visual). Delirium tremens <strong>of</strong>ten follows after withdrawal<br />
seizures <strong>and</strong> is a medical emergency. If untreated,<br />
death may occur as a result <strong>of</strong> respiratory or cardiovascular<br />
collapse. Management includes thiamine <strong>and</strong> other vitamin<br />
replacement, <strong>and</strong> a long-acting oral benzodiazepines (e.g.<br />
chlordiazepoxide or diazepam), given by mouth if possible.<br />
The initial dose requirement is determined empirically <strong>and</strong> is<br />
followed by a regimen <strong>of</strong> step-wise dose reduction over the<br />
CENTRAL DEPRESSANTS 441<br />
next two to three days. The patient should be nursed in a quiet<br />
environment with careful attention to fluid <strong>and</strong> electrolyte<br />
balance. Benzodiazepines (intravenous if necessary, Chapters<br />
18 <strong>and</strong> 22) are usually effective in terminating prolonged withdrawal<br />
seizures – if they are ineffective the diagnosis should<br />
be reconsidered (e.g. is there evidence <strong>of</strong> intracranial haemorrhage<br />
or infection). Psychiatric assessment <strong>and</strong> social support<br />
are indicated once the withdrawal syndrome has receded.<br />
Key points<br />
Delirium tremens<br />
• Mortality is 5–10%.<br />
• There is a state <strong>of</strong> acute confusion <strong>and</strong> disorientation<br />
associated with frightening hallucinations <strong>and</strong><br />
sympathetic overactivity. Delirium tremens occurs in less<br />
than 10% <strong>of</strong> alcoholic patients withdrawing from<br />
alcohol.<br />
• Management includes:<br />
– nursing in a quiet, evenly illuminated room;<br />
– sedation (either clomethiazole or diazepam);<br />
– vitamin replacement with adequate thiamine;<br />
– correction <strong>of</strong> fluid <strong>and</strong> electrolyte balance;<br />
– psychiatric referral.<br />
Long-term management <strong>of</strong> the alcoholic<br />
Psychological <strong>and</strong> social management: Some form <strong>of</strong><br />
psychological <strong>and</strong> social management is important to help<br />
the patient to remain abstinent. Whatever approach is used,<br />
the focus has to be on abstinence from alcohol. A very small<br />
minority <strong>of</strong> patients may be able to take up controlled<br />
drinking subsequently, but it is impossible to identify this<br />
group prospectively, <strong>and</strong> this should not be a goal <strong>of</strong><br />
treatment. Voluntary agencies such as Alcoholics<br />
Anonymous are useful resources <strong>and</strong> patients should be<br />
encouraged to attend them.<br />
Alcohol-sensitizing drugs: These produce an unpleasant<br />
reaction when taken with alcohol. The only drug <strong>of</strong> this type<br />
used to treat alcoholics is disulfiram, which inhibits aldehyde<br />
dehydrogenase, leading to acetaldehyde accumulation if<br />
alcohol is taken, causing flushing, sweating, nausea,<br />
headache, tachycardia <strong>and</strong> hypotension. Cardiac dysrhythmias<br />
may occur if large amounts <strong>of</strong> alcohol are consumed. The<br />
small amounts <strong>of</strong> alcohol included in many medicines may be<br />
sufficient to produce a reaction <strong>and</strong> it is advisable for the<br />
patient to carry a card warning <strong>of</strong> the danger <strong>of</strong> alcohol<br />
administration. Disulfiram also inhibits phenytoin<br />
metabolism <strong>and</strong> can lead to phenytoin intoxication.<br />
Unfortunately, there is only weak evidence that disulfiram<br />
has any benefit in the treatment <strong>of</strong> alcoholism. Its use should<br />
be limited to highly selected individuals in specialist clinics.<br />
Acamprosate: The structure <strong>of</strong> acamprosate resembles that <strong>of</strong><br />
GABA <strong>and</strong> glutamate. It appears to reduce the effects <strong>of</strong><br />
excitatory amino acids <strong>and</strong>, combined with counselling, it<br />
may help to maintain abstinence after alcohol withdrawal.