A Textbook of Clinical Pharmacology and Therapeutics
A Textbook of Clinical Pharmacology and Therapeutics
A Textbook of Clinical Pharmacology and Therapeutics
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
one marrow to produce red cells. The only advantages <strong>of</strong><br />
parenteral iron are the following:<br />
• Iron stores are rapidly <strong>and</strong> completely replenished.<br />
• There is no doubt about compliance.<br />
• It is effective in patients with malabsorption.<br />
Parenteral iron should therefore only be considered in the<br />
following situations:<br />
• malabsorption;<br />
• genuine intolerance <strong>of</strong> oral iron preparations;<br />
• when continued blood loss is not preventable <strong>and</strong> large<br />
doses <strong>of</strong> iron cannot be readily given by mouth;<br />
• failure <strong>of</strong> patient compliance;<br />
• when great dem<strong>and</strong>s are to be made on a patient’s iron<br />
stores (e.g. in an anaemic pregnant woman just before term).<br />
IRON DEXTRAN AND IRON SUCROSE INJECTIONS<br />
Use<br />
These can be administered by deep intramuscular injection (to<br />
minimize staining <strong>of</strong> the skin) or intravenously (anaphylactoid<br />
reactions can occur (up 3% <strong>of</strong> patients) <strong>and</strong> a small test dose<br />
should be given initially). Oral iron should be stopped 24<br />
hours before starting parenteral iron therapy <strong>and</strong> not restarted<br />
until five days after the last injection.<br />
Key points<br />
Iron replacement therapy<br />
• In health, normal iron losses require the absorption <strong>of</strong><br />
0.5–1 mg (in males) <strong>and</strong> 0.7–2 mg (in menstruating<br />
females) <strong>of</strong> iron.<br />
• Ferrous iron is best absorbed from the small intestine.<br />
• Iron deficiency is the most common cause <strong>of</strong> anaemia<br />
(e.g. malabsorption, menstrual, occult or gastrointestinal<br />
blood loss – always determine the cause).<br />
• For iron deficiency, 100–200 mg <strong>of</strong> elemental iron<br />
are given orally per day <strong>and</strong> continued until iron stores<br />
are replete, usually within three to six months.<br />
• Parenteral iron use is restricted to cases <strong>of</strong> noncompliance<br />
or non-tolerance <strong>of</strong> oral preparations,<br />
or malabsorption states.<br />
• During erythropoietin therapy, supplemental iron is<br />
given to support increased haem synthesis.<br />
VITAMIN B 12<br />
Vitamin B 12 is an organic molecule with an attached cobalt<br />
atom. Linked to the cobalt atom may be a cyanide (cyanocobalamin),<br />
hydroxyl (hydroxocobalamin) or methyl (methylcobalamin)<br />
group. These forms are interconvertible. Sources <strong>of</strong><br />
vitamin B 12 include liver, kidney heart, fish <strong>and</strong> eggs.<br />
Use<br />
Replacement therapy is required in vitamin B12 deficiency<br />
which may be due to:<br />
• malabsorption secondary to gastric pathology (Addisonian<br />
pernicious anaemia, where parietal cells are destroyed by an<br />
HAEMATINICS – IRON, VITAMIN B 12 AND FOLATE 391<br />
autoimmune reaction, so intrinsic factor is not produced,<br />
resulting in vitamin B 12 deficiency; gastrectomy);<br />
• intestinal malabsorption (e.g. Crohn’s disease or surgical<br />
resection <strong>of</strong> the terminal ileum);<br />
• competition for vitamin B 12 absorption by gut organisms<br />
(e.g. blind loop syndrome due to a jejunal diverticulum or<br />
other cause <strong>of</strong> bacterial overgrowth, infestation with the<br />
fish tapeworm Diphyllobothrium latum);<br />
• nutritional deficiency – this is rare <strong>and</strong> is limited to strict<br />
vegans. The few such individuals who do develop<br />
megaloblastic anaemia <strong>of</strong>ten have some co-existing<br />
deficiency <strong>of</strong> intrinsic factor.<br />
Vitamin B 12 replacement therapy is given by intramuscular<br />
injection. Hydroxocobalamin is preferred, given as an initial<br />
loading dose followed by three monthly maintenance treatment<br />
for life.<br />
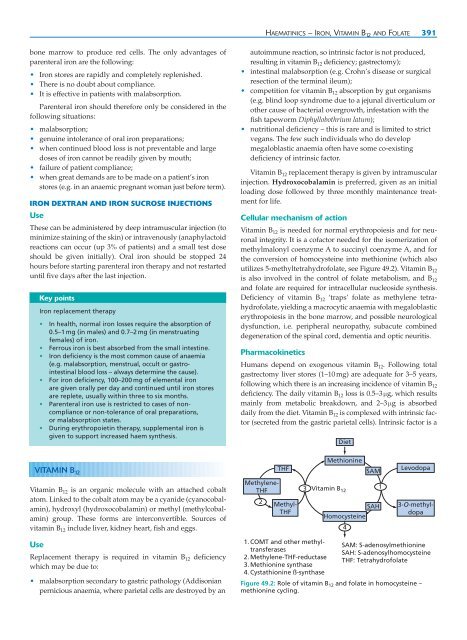
Cellular mechanism <strong>of</strong> action<br />
Vitamin B12 is needed for normal erythropoiesis <strong>and</strong> for neuronal<br />
integrity. It is a c<strong>of</strong>actor needed for the isomerization <strong>of</strong><br />
methylmalonyl coenzyme A to succinyl coenzyme A, <strong>and</strong> for<br />
the conversion <strong>of</strong> homocysteine into methionine (which also<br />
utilizes 5-methyltetrahydr<strong>of</strong>olate, see Figure 49.2). Vitamin B12 is also involved in the control <strong>of</strong> folate metabolism, <strong>and</strong> B12 <strong>and</strong> folate are required for intracellular nucleoside synthesis.<br />
Deficiency <strong>of</strong> vitamin B12 ‘traps’ folate as methylene tetrahydr<strong>of</strong>olate,<br />
yielding a macrocytic anaemia with megaloblastic<br />
erythropoiesis in the bone marrow, <strong>and</strong> possible neurological<br />
dysfunction, i.e. peripheral neuropathy, subacute combined<br />
degeneration <strong>of</strong> the spinal cord, dementia <strong>and</strong> optic neuritis.<br />
Pharmacokinetics<br />
Humans depend on exogenous vitamin B12. Following total<br />
gastrectomy liver stores (1–10 mg) are adequate for 3–5 years,<br />
following which there is an increasing incidence <strong>of</strong> vitamin B12 deficiency. The daily vitamin B12 loss is 0.5–3 μg, which results<br />
mainly from metabolic breakdown, <strong>and</strong> 2–3 μg is absorbed<br />
daily from the diet. Vitamin B12 is complexed with intrinsic factor<br />
(secreted from the gastric parietal cells). Intrinsic factor is a<br />
Methylene-<br />
THF<br />
2<br />
THF<br />
Methyl-<br />
THF<br />
1. COMT <strong>and</strong> other methyltransferases<br />
2. Methylene-THF-reductase<br />
3. Methionine synthase<br />
4. Cystathionine ß-synthase<br />
3<br />
Diet<br />
Methionine<br />
Vitamin B 12<br />
SAM<br />
SAH<br />
Homocysteine<br />
4<br />
1<br />
Levodopa<br />
3-O-methyldopa<br />
SAM: S-adenosylmethionine<br />
SAH: S-adenosylhomocysteine<br />
THF: Tetrahydr<strong>of</strong>olate<br />
Figure 49.2: Role <strong>of</strong> vitamin B 12 <strong>and</strong> folate in homocysteine –<br />
methionine cycling.