A Textbook of Clinical Pharmacology and Therapeutics
A Textbook of Clinical Pharmacology and Therapeutics
A Textbook of Clinical Pharmacology and Therapeutics
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
36 EFFECTS OF DISEASE ON DRUG DISPOSITION<br />
<strong>and</strong> other plasma proteins. This alters the pharmacokinetics <strong>of</strong><br />
many drugs, but is seldom clinically important. Phenytoin<br />
is an exception, because therapy is guided by plasma concentration<br />
<strong>and</strong> routine analytical methods detect total (bound<br />
<strong>and</strong> free) drug. In renal impairment, phenytoin protein binding<br />
is reduced by competition with accumulated molecules<br />
normally cleared by the kidney <strong>and</strong> which bind to the same<br />
albumin drug-binding site as phenytoin. Thus, for any measured<br />
phenytoin concentration, free (active) drug is increased<br />
compared to a subject with normal renal function <strong>and</strong> the<br />
same measured total concentration. The therapeutic range<br />
therefore has to be adjusted to lower values in patients with<br />
renal impairment, as otherwise doses will be selected that<br />
cause toxicity.<br />
Tissue binding <strong>of</strong> digoxin is reduced in patients with<br />
impaired renal function, resulting in a lower volume <strong>of</strong> distribution<br />
than in healthy subjects. A reduced loading dose <strong>of</strong><br />
digoxin is therefore appropriate in such patients, although the<br />
effect <strong>of</strong> reduced glomerular filtration on digoxin clearance is<br />
even more important, necessitating a reduced maintenance<br />
dose, as described below.<br />
The blood–brain barrier is more permeable to drugs in<br />
uraemia. This can result in increased access <strong>of</strong> drugs to the<br />
central nervous system, an effect that is believed to contribute<br />
to the increased incidence <strong>of</strong> confusion caused by cimetidine,<br />
ranitidine <strong>and</strong> famotidine in patients with renal failure.<br />
METABOLISM<br />
Metabolism <strong>of</strong> several drugs is reduced in renal failure. These<br />
include drugs that undergo phase I metabolism by CYP3A4.<br />
Drugs that are mainly metabolized by phase II drug metabolism<br />
are less affected, although conversion <strong>of</strong> sulindac to its<br />
active sulphide metabolite is impaired in renal failure, as is the<br />
hepatic conjugation <strong>of</strong> metoclopramide with glucuronide <strong>and</strong><br />
sulphate.<br />
RENAL EXCRETION<br />
Glomerular filtration <strong>and</strong> tubular secretion <strong>of</strong> drugs usually<br />
fall in step with one another in patients with renal impairment.<br />
Drug excretion is directly related to glomerular filtration<br />
rate (GFR). Some estimate <strong>of</strong> GFR (eGFR) is therefore<br />
essential when deciding on an appropriate dose regimen.<br />
Serum creatinine concentration adjusted for age permits calculation<br />
<strong>of</strong> an estimate <strong>of</strong> GFR per 1.73 m2 body surface area.<br />
This is now provided by most chemical pathology laboratories,<br />
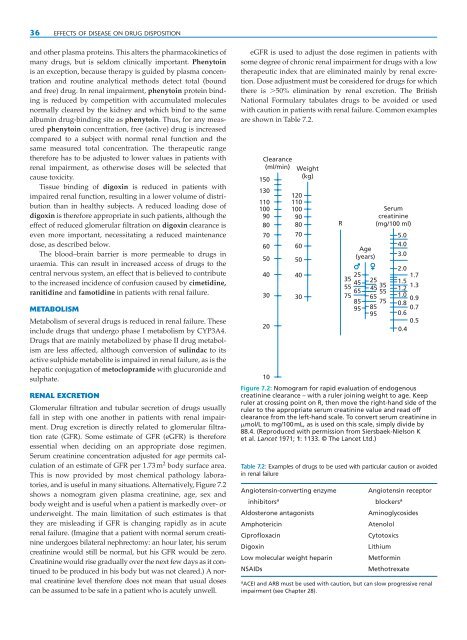
<strong>and</strong> is useful in many situations. Alternatively, Figure 7.2<br />
shows a nomogram given plasma creatinine, age, sex <strong>and</strong><br />
body weight <strong>and</strong> is useful when a patient is markedly over- or<br />
underweight. The main limitation <strong>of</strong> such estimates is that<br />
they are misleading if GFR is changing rapidly as in acute<br />
renal failure. (Imagine that a patient with normal serum creatinine<br />
undergoes bilateral nephrectomy: an hour later, his serum<br />
creatinine would still be normal, but his GFR would be zero.<br />
Creatinine would rise gradually over the next few days as it continued<br />
to be produced in his body but was not cleared.) A normal<br />
creatinine level therefore does not mean that usual doses<br />
can be assumed to be safe in a patient who is acutely unwell.<br />
eGFR is used to adjust the dose regimen in patients with<br />
some degree <strong>of</strong> chronic renal impairment for drugs with a low<br />
therapeutic index that are eliminated mainly by renal excretion.<br />
Dose adjustment must be considered for drugs for which<br />
there is �50% elimination by renal excretion. The British<br />
National Formulary tabulates drugs to be avoided or used<br />
with caution in patients with renal failure. Common examples<br />
are shown in Table 7.2.<br />
Clearance<br />
(ml/min) Weight<br />
150<br />
(kg)<br />
130<br />
110<br />
100<br />
90<br />
80<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
120<br />
110<br />
100<br />
90<br />
80<br />
70<br />
60<br />
50<br />
40<br />
30<br />
R<br />
Age<br />
(years)<br />
25<br />
35<br />
45<br />
25<br />
55<br />
65<br />
45<br />
35<br />
55<br />
75 65<br />
85 75<br />
95 85<br />
95<br />
Serum<br />
creatinine<br />
(mg/100 ml)<br />
5.0<br />
4.0<br />
3.0<br />
2.0<br />
1.7<br />
1.5<br />
1.2<br />
1.3<br />
1.0<br />
0.9<br />
0.8<br />
0.7<br />
0.6<br />
0.5<br />
0.4<br />
10<br />
Figure 7.2: Nomogram for rapid evaluation <strong>of</strong> endogenous<br />
creatinine clearance – with a ruler joining weight to age. Keep<br />
ruler at crossing point on R, then move the right-h<strong>and</strong> side <strong>of</strong> the<br />
ruler to the appropriate serum creatinine value <strong>and</strong> read <strong>of</strong>f<br />
clearance from the left-h<strong>and</strong> scale. To convert serum creatinine in<br />
�mol/L to mg/100mL, as is used on this scale, simply divide by<br />
88.4. (Reproduced with permission from Siersbaek-Nielson K<br />
et al. Lancet 1971; 1: 1133. © The Lancet Ltd.)<br />
Table 7.2: Examples <strong>of</strong> drugs to be used with particular caution or avoided<br />
in renal failure<br />
Angiotensin-converting enzyme Angiotensin receptor<br />
inhibitorsa blockersa Aldosterone antagonists Aminoglycosides<br />
Amphotericin Atenolol<br />
Cipr<strong>of</strong>loxacin Cytotoxics<br />
Digoxin Lithium<br />
Low molecular weight heparin Metformin<br />
NSAIDs Methotrexate<br />
aACEI <strong>and</strong> ARB must be used with caution, but can slow progressive renal<br />
impairment (see Chapter 28).