A Textbook of Clinical Pharmacology and Therapeutics
A Textbook of Clinical Pharmacology and Therapeutics
A Textbook of Clinical Pharmacology and Therapeutics
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
or with potassium-sparing diuretics (see above). Hyperkalaemia<br />
is particularly likely to occur in patients with<br />
impaired renal function, in the elderly (in whom renal impairment<br />
may be unrecognized because the plasma creatinine concentration<br />
is normal) <strong>and</strong> in patients receiving ACE inhibitors,<br />
K � supplements or NSAID.<br />
Treatment<br />
1. Calcium gluconate is a potentially life-saving emergency<br />
treatment in patients with dysrhythmias caused by<br />
hyperkalaemia (Chapter 32). It is given intravenously<br />
with ECG monitoring.<br />
2. Glucose <strong>and</strong> insulin shift extracellular K� into cells.<br />
3. Sodium bicarbonate, given intravenously, also shifts K� into cells.<br />
4. High-dose nebulized β2-agonists shift K� into cells.<br />
5. Ion-exchange resin made <strong>of</strong> sodium or calcium<br />
polystyrene sulphonate removes potassium from the body<br />
in stool. The main adverse effect when resins are given<br />
chronically for patients with chronic renal failure is<br />
constipation, which can be avoided if the resins are<br />
suspended in a solution <strong>of</strong> sorbitol.<br />
6. Emergency haem<strong>of</strong>iltration or dialysis.<br />
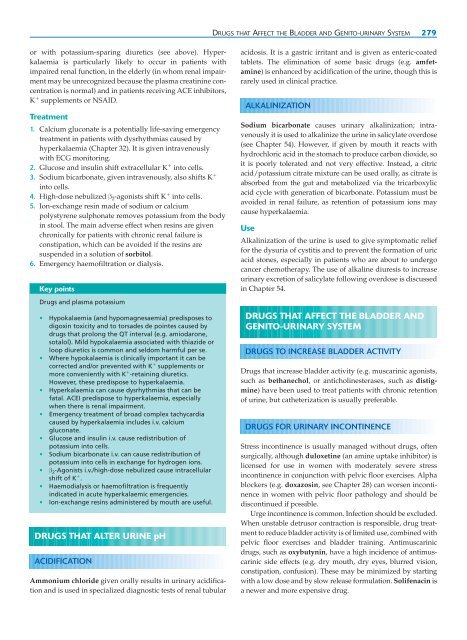
Key points<br />
Drugs <strong>and</strong> plasma potassium<br />
• Hypokalaemia (<strong>and</strong> hypomagnesaemia) predisposes to<br />
digoxin toxicity <strong>and</strong> to torsades de pointes caused by<br />
drugs that prolong the QT interval (e.g. amiodarone,<br />
sotalol). Mild hypokalaemia associated with thiazide or<br />
loop diuretics is common <strong>and</strong> seldom harmful per se.<br />
• Where hypokalaemia is clinically important it can be<br />
corrected <strong>and</strong>/or prevented with K � supplements or<br />
more conveniently with K � -retaining diuretics.<br />
However, these predispose to hyperkalaemia.<br />
• Hyperkalaemia can cause dysrhythmias that can be<br />
fatal. ACEI predispose to hyperkalaemia, especially<br />
when there is renal impairment.<br />
• Emergency treatment <strong>of</strong> broad complex tachycardia<br />
caused by hyperkalaemia includes i.v. calcium<br />
gluconate.<br />
• Glucose <strong>and</strong> insulin i.v. cause redistribution <strong>of</strong><br />
potassium into cells.<br />
• Sodium bicarbonate i.v. can cause redistribution <strong>of</strong><br />
potassium into cells in exchange for hydrogen ions.<br />
• β 2-Agonists i.v./high-dose nebulized cause intracellular<br />
shift <strong>of</strong> K � .<br />
• Haemodialysis or haem<strong>of</strong>iltration is frequently<br />
indicated in acute hyperkalaemic emergencies.<br />
• Ion-exchange resins administered by mouth are useful.<br />
DRUGS THAT ALTER URINE pH<br />
ACIDIFICATION<br />
Ammonium chloride given orally results in urinary acidification<br />
<strong>and</strong> is used in specialized diagnostic tests <strong>of</strong> renal tubular<br />
DRUGS THAT AFFECT THE BLADDER AND GENITO-URINARY SYSTEM 279<br />
acidosis. It is a gastric irritant <strong>and</strong> is given as enteric-coated<br />
tablets. The elimination <strong>of</strong> some basic drugs (e.g. amfetamine)<br />
is enhanced by acidification <strong>of</strong> the urine, though this is<br />
rarely used in clinical practice.<br />
ALKALINIZATION<br />
Sodium bicarbonate causes urinary alkalinization; intravenously<br />
it is used to alkalinize the urine in salicylate overdose<br />
(see Chapter 54). However, if given by mouth it reacts with<br />
hydrochloric acid in the stomach to produce carbon dioxide, so<br />
it is poorly tolerated <strong>and</strong> not very effective. Instead, a citric<br />
acid/potassium citrate mixture can be used orally, as citrate is<br />
absorbed from the gut <strong>and</strong> metabolized via the tricarboxylic<br />
acid cycle with generation <strong>of</strong> bicarbonate. Potassium must be<br />
avoided in renal failure, as retention <strong>of</strong> potassium ions may<br />
cause hyperkalaemia.<br />
Use<br />
Alkalinization <strong>of</strong> the urine is used to give symptomatic relief<br />
for the dysuria <strong>of</strong> cystitis <strong>and</strong> to prevent the formation <strong>of</strong> uric<br />
acid stones, especially in patients who are about to undergo<br />
cancer chemotherapy. The use <strong>of</strong> alkaline diuresis to increase<br />
urinary excretion <strong>of</strong> salicylate following overdose is discussed<br />
in Chapter 54.<br />
DRUGS THAT AFFECT THE BLADDER AND<br />
GENITO-URINARY SYSTEM<br />
DRUGS TO INCREASE BLADDER ACTIVITY<br />
Drugs that increase bladder activity (e.g. muscarinic agonists,<br />
such as bethanechol, or anticholinesterases, such as distigmine)<br />
have been used to treat patients with chronic retention<br />
<strong>of</strong> urine, but catheterization is usually preferable.<br />
DRUGS FOR URINARY INCONTINENCE<br />
Stress incontinence is usually managed without drugs, <strong>of</strong>ten<br />
surgically, although duloxetine (an amine uptake inhibitor) is<br />
licensed for use in women with moderately severe stress<br />
incontinence in conjunction with pelvic floor exercises. Alpha<br />
blockers (e.g. doxazosin, see Chapter 28) can worsen incontinence<br />
in women with pelvic floor pathology <strong>and</strong> should be<br />
discontinued if possible.<br />
Urge incontinence is common. Infection should be excluded.<br />
When unstable detrusor contraction is responsible, drug treatment<br />
to reduce bladder activity is <strong>of</strong> limited use, combined with<br />
pelvic floor exercises <strong>and</strong> bladder training. Antimuscarinic<br />
drugs, such as oxybutynin, have a high incidence <strong>of</strong> antimuscarinic<br />
side effects (e.g. dry mouth, dry eyes, blurred vision,<br />
constipation, confusion). These may be minimized by starting<br />
with a low dose <strong>and</strong> by slow release formulation. Solifenacin is<br />
a newer <strong>and</strong> more expensive drug.