Health Inequities in Manitoba: Is the Socioeconomic Gap
Health Inequities in Manitoba: Is the Socioeconomic Gap
Health Inequities in Manitoba: Is the Socioeconomic Gap
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Health</strong> <strong>Inequities</strong> <strong>in</strong> <strong>Manitoba</strong>: <strong>Is</strong> <strong>the</strong> <strong>Socioeconomic</strong> <strong>Gap</strong> <strong>in</strong> <strong>Health</strong> Widen<strong>in</strong>g or Narrow<strong>in</strong>g Over Time?<br />
• 8496—regional gynaecological exam, <strong>in</strong>clud<strong>in</strong>g cytological smear of <strong>the</strong> cervix, provided by an<br />
OB/GYN specialist<br />
• 8498—complete physical and gynaecological exam, <strong>in</strong>clud<strong>in</strong>g cytological smear of <strong>the</strong> cervix,<br />
provided by a GP/FP<br />
• 9795—cytological smear of <strong>the</strong> cervix for cancer screen<strong>in</strong>g<br />
• A pathology or laboratory claim with a tariff code for a Pap test:<br />
• 9470—Cytological Exam<strong>in</strong>ation—Vag<strong>in</strong>al Smear<br />
The denom<strong>in</strong>ator <strong>in</strong>cludes all <strong>Manitoba</strong> female residents aged 18–69 <strong>in</strong> <strong>the</strong> three–year period, except as<br />
noted below.<br />
Note that if a laboratory claim and a physician claim for a Pap test for <strong>the</strong> same <strong>in</strong>dividual are with<strong>in</strong> 54<br />
days of each o<strong>the</strong>r, <strong>the</strong>y are counted as one Pap test to reduce double count<strong>in</strong>g over three–year periods.<br />
Nearly all of lab claims are with<strong>in</strong> 54 days of <strong>the</strong> physician claim.<br />
Women who have had a complete hysterectomy surgery were excluded from both <strong>the</strong> numerator and<br />
denom<strong>in</strong>ator. Hysterectomy surgeries were def<strong>in</strong>ed by hospital separations with ICD–9–CM procedure<br />
codes 68.4–68.9 and ICD–10–CCI codes 1.RM.89, 1.RM.91, 5.CA.89.CK, 5.CA.89.DA, 5.CA.89.GB, 5.CA.89.<br />
WJ, and 5.CA.89.WK. These codes <strong>in</strong>clude only total hysterectomies, not partial, as women who have a<br />
partial hysterectomy may still have a cervix and would require cervical cancer screen<strong>in</strong>g.<br />
Rates for nor<strong>the</strong>rn and remote areas served by nurs<strong>in</strong>g stations may be underestimated due to miss<strong>in</strong>g<br />
data. Prior to 2005, only physicians were able to code <strong>in</strong>to <strong>the</strong> adm<strong>in</strong>istrative bill<strong>in</strong>g system for Pap tests.<br />
As of 2005, nurses officially called “Nurse Practitioners” by <strong>Manitoba</strong> <strong>Health</strong> were able to record claims <strong>in</strong><br />
<strong>the</strong> physician data system. However, “Advanced Practice Nurses” or o<strong>the</strong>r designations are not <strong>in</strong>cluded<br />
<strong>in</strong> <strong>the</strong> Nurse Practitioner designation, despite <strong>the</strong> fact that some do Pap tests. Nurses work<strong>in</strong>g at<br />
federally–operated Nurs<strong>in</strong>g Stations also do not record <strong>the</strong>ir work <strong>in</strong> <strong>the</strong> bill<strong>in</strong>g claims system. However,<br />
most nurses who are not nurse practitioners would be do<strong>in</strong>g Pap tests under <strong>the</strong> supervision of a<br />
physician, who would most likely be bill<strong>in</strong>g for <strong>the</strong>se. At <strong>the</strong> time of this study, <strong>the</strong> Repository at MCHP<br />
did not have access to laboratory data, so Pap tests are only observable through <strong>the</strong> bill<strong>in</strong>g system.<br />
Cont<strong>in</strong>uity of Care<br />
The extent to which <strong>in</strong>dividuals see a given healthcare provider (versus one or more o<strong>the</strong>r providers)<br />
over a two–year period. In this study, ‘good’ cont<strong>in</strong>uity of care is when a resident receives at least 50%<br />
of his or her ambulatory care from <strong>the</strong> same healthcare provider over <strong>the</strong> time period. A provider may<br />
be def<strong>in</strong>ed ei<strong>the</strong>r as an <strong>in</strong>dividual physician, a physician group practice, or a cl<strong>in</strong>ic. Individuals with less<br />
than three visits to a healthcare provider were excluded from analyses. Tables describ<strong>in</strong>g <strong>the</strong> proportion<br />
of <strong>the</strong> population excluded from <strong>the</strong>se analyses are below.<br />
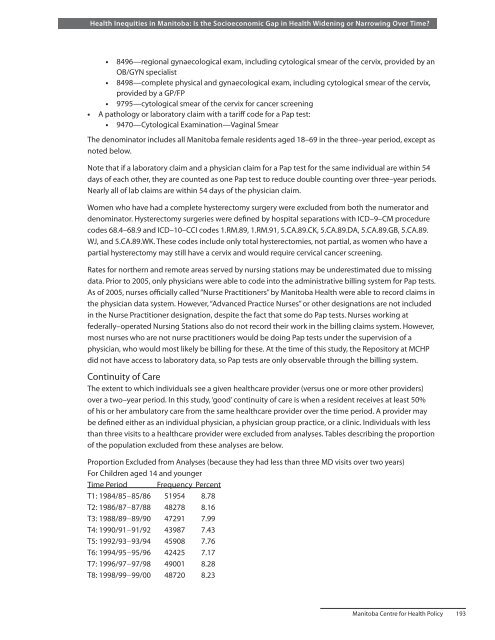
Proportion Excluded from Analyses (because <strong>the</strong>y had less than three MD visits over two years)<br />
For Children aged 14 and younger<br />
Time Period Frequency Percent<br />
T1: 1984/85–85/86 51954 8.78<br />
T2: 1986/87–87/88 48278 8.16<br />
T3: 1988/89–89/90 47291 7.99<br />
T4: 1990/91–91/92 43987 7.43<br />
T5: 1992/93–93/94 45908 7.76<br />
T6: 1994/95–95/96 42425 7.17<br />
T7: 1996/97–97/98 49001 8.28<br />
T8: 1998/99–99/00 48720 8.23<br />
<strong>Manitoba</strong> Centre for <strong>Health</strong> Policy 193