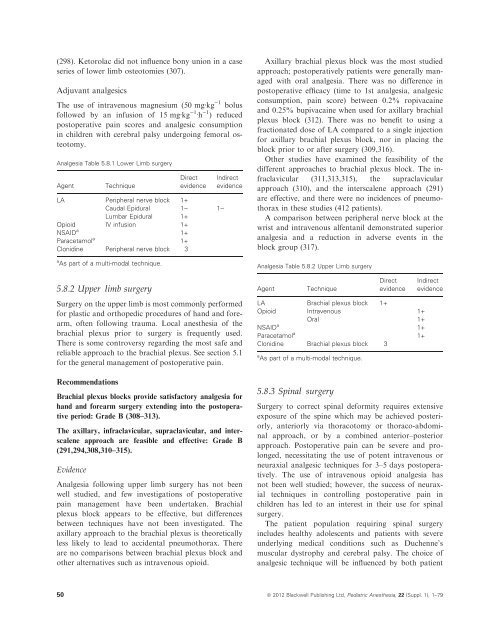
(298). Ketorolac did not <strong>in</strong>fluence bony union <strong>in</strong> a caseseries of lower limb osteotomies (307).Adjuvant analgesicsThe use of <strong>in</strong>travenous magnesium (50 mgÆkg )1 bolusfollowed by an <strong>in</strong>fusion of 15 mgÆkg )1 Æh )1 ) reducedpostoperative pa<strong>in</strong> scores <strong>and</strong> analgesic consumption<strong>in</strong> children with cerebral palsy undergo<strong>in</strong>g femoral osteotomy.Analgesia Table 5.8.1 Lower Limb surgeryAgentTechniqueDirectevidenceLA Peripheral nerve block 1+Caudal Epidural 1) 1)Lumbar Epidural 1+Opioid IV <strong>in</strong>fusion 1+NSAID a 1+Paracetamol a 1+Clonid<strong>in</strong>e Peripheral nerve block 3a As part of a multi-modal technique.IndirectevidenceAxillary brachial plexus block was the most studiedapproach; postoperatively patients were generally managedwith oral analgesia. There was no difference <strong>in</strong>postoperative efficacy (time to 1st analgesia, analgesicconsumption, pa<strong>in</strong> score) between 0.2% ropivaca<strong>in</strong>e<strong>and</strong> 0.25% bupivaca<strong>in</strong>e when used for axillary brachialplexus block (312). There was no benefit to us<strong>in</strong>g afractionated dose of LA compared to a s<strong>in</strong>gle <strong>in</strong>jectionfor axillary brachial plexus block, nor <strong>in</strong> plac<strong>in</strong>g theblock prior to or after surgery (309,316).Other studies have exam<strong>in</strong>ed the feasibility of thedifferent approaches to brachial plexus block. The <strong>in</strong>fraclavicular(311,313,315), the supraclavicularapproach (310), <strong>and</strong> the <strong>in</strong>terscalene approach (291)are effective, <strong>and</strong> there were no <strong>in</strong>cidences of pneumothorax<strong>in</strong> these studies (412 patients).A comparison between peripheral nerve block at thewrist <strong>and</strong> <strong>in</strong>travenous alfentanil demonstrated superioranalgesia <strong>and</strong> a reduction <strong>in</strong> adverse events <strong>in</strong> theblock group (317).Analgesia Table 5.8.2 Upper Limb surgery5.8.2 Upper limb surgeryAgentTechniqueDirectevidenceIndirectevidenceSurgery on the upper limb is most commonly performedfor plastic <strong>and</strong> orthopedic procedures of h<strong>and</strong> <strong>and</strong> forearm,often follow<strong>in</strong>g trauma. Local anesthesia of thebrachial plexus prior to surgery is frequently used.There is some controversy regard<strong>in</strong>g the most safe <strong>and</strong>reliable approach to the brachial plexus. See section 5.1for the general management of postoperative pa<strong>in</strong>.RecommendationsBrachial plexus blocks provide satisfactory analgesia forh<strong>and</strong> <strong>and</strong> forearm surgery extend<strong>in</strong>g <strong>in</strong>to the postoperativeperiod: Grade B (308–313).The axillary, <strong>in</strong>fraclavicular, supraclavicular, <strong>and</strong> <strong>in</strong>terscaleneapproach are feasible <strong>and</strong> effective: Grade B(291,294,308,310–315).EvidenceAnalgesia follow<strong>in</strong>g upper limb surgery has not beenwell studied, <strong>and</strong> few <strong>in</strong>vestigations of postoperativepa<strong>in</strong> management have been undertaken. Brachialplexus block appears to be effective, but differencesbetween techniques have not been <strong>in</strong>vestigated. Theaxillary approach to the brachial plexus is theoreticallyless likely to lead to accidental pneumothorax. Thereare no comparisons between brachial plexus block <strong>and</strong>other alternatives such as <strong>in</strong>travenous opioid.LA Brachial plexus block 1+Opioid Intravenous 1+Oral 1+NSAID a 1+Paracetamol a 1+Clonid<strong>in</strong>e Brachial plexus block 3a As part of a multi-modal technique.5.8.3 Sp<strong>in</strong>al surgerySurgery to correct sp<strong>in</strong>al deformity requires extensiveexposure of the sp<strong>in</strong>e which may be achieved posteriorly,anteriorly via thoracotomy or thoraco-abdom<strong>in</strong>alapproach, or by a comb<strong>in</strong>ed anterior–posteriorapproach. <strong>Postoperative</strong> pa<strong>in</strong> can be severe <strong>and</strong> prolonged,necessitat<strong>in</strong>g the use of potent <strong>in</strong>travenous orneuraxial analgesic techniques for 3–5 days postoperatively.The use of <strong>in</strong>travenous opioid analgesia hasnot been well studied; however, the success of neuraxialtechniques <strong>in</strong> controll<strong>in</strong>g postoperative pa<strong>in</strong> <strong>in</strong>children has led to an <strong>in</strong>terest <strong>in</strong> their use for sp<strong>in</strong>alsurgery.The patient population requir<strong>in</strong>g sp<strong>in</strong>al surgery<strong>in</strong>cludes healthy adolescents <strong>and</strong> patients with severeunderly<strong>in</strong>g medical conditions such as Duchenne’smuscular dystrophy <strong>and</strong> cerebral palsy. The choice ofanalgesic technique will be <strong>in</strong>fluenced by both patient50 ª 2012 Blackwell Publish<strong>in</strong>g Ltd, Pediatric Anesthesia, 22 (Suppl. 1), 1–79
<strong>and</strong> surgical factors <strong>in</strong> addition to local circumstances,for example, neuraxial techniques are not suitable forsome patients. The <strong>in</strong>volvement of the surgeon <strong>in</strong> thechoice of analgesic technique is especially important <strong>in</strong>sp<strong>in</strong>al surgery as it must also enable early <strong>and</strong> frequentassessment of neurological function, <strong>and</strong> epidural LAis not usually adm<strong>in</strong>istered follow<strong>in</strong>g surgery until normalneurological function has been demonstrated. Seesection 5.1 for the general management of postoperativepa<strong>in</strong>.<strong>Good</strong> practice po<strong>in</strong>tThere is no evidence from studies <strong>in</strong> children thatNSAIDs have a deleterious effect on bone fusion. Theanalgesic benefit of short-term NSAID use has beendemonstrated <strong>and</strong> may frequently outweigh any hypotheticalrisk.RecommendationsEpidural techniques produce a modest improvement <strong>in</strong>pa<strong>in</strong> control, compared with <strong>in</strong>travenous opioids <strong>in</strong>patients undergo<strong>in</strong>g corrective surgery for adolescent idiopathicscoliosis: Grade B (318–322).Intrathecal opioids decrease <strong>in</strong>tra-operative blood loss<strong>and</strong> IV opioid consumption postoperatively. The durationof action is 18–24 h: Grade C (318,323–326).Dual catheter epidural techniques should be considered,as this permits coverage of multiple sp<strong>in</strong>al levels: GradeC (319,327–329).The use of LA + lipophilic opioid <strong>in</strong> the epidural spacewith a s<strong>in</strong>gle epidural catheter does not show an analgesicbenefit over <strong>in</strong>travenous opioid techniques: Grade C(330,331).The use of LA + hydrophilic opioids <strong>in</strong> the epiduralspace has a favorable analgesic profile compared withIV opioid, but at the expense of <strong>in</strong>crease adverse effects:Grade D (332,333).EvidenceThe majority of studies have been conducted <strong>in</strong> adolescents,<strong>and</strong> some studies have also <strong>in</strong>cluded young adultsup to the age of 22 years. Neuraxial techniques havebeen the most <strong>in</strong>vestigated. Intrathecal (IT) opioids: s<strong>in</strong>gledoses of IT opioids can reduce <strong>in</strong>traoperative bloodloss <strong>and</strong> postoperative analgesic requirements. IT morph<strong>in</strong>eplus sufentanil decreased <strong>in</strong>tra-operative bloodloss compared with IV sufentanil (323). IT morph<strong>in</strong>e5 lgÆkg )1 also decreased <strong>in</strong>tra-operative blood losscompared with 2 lgÆkg )1 IT or sal<strong>in</strong>e controls (324).The time to first analgesic use, 6–24 h postoperatively,was significantly <strong>in</strong>creased <strong>in</strong> proportion to dose of ITmorph<strong>in</strong>e <strong>in</strong> these studies (323,324,334). Pa<strong>in</strong> scoreswere also lower with <strong>in</strong>trathecal morph<strong>in</strong>e (318,324).However, the use of a high-dose <strong>in</strong>trathecal opioidregime (15 lgÆkg )1 morph<strong>in</strong>e + 1 lgÆkg )1 sufentanil)did not improve analgesic efficacy or enhance the reduction<strong>in</strong> blood loss compared with a low-dose regimen(5 lgÆkg )1 morph<strong>in</strong>e + 1 lgÆkg )1 sufentanil) (325).Several studies have found no <strong>in</strong>crease <strong>in</strong> respiratorydepression with IT opioids up to a maximum dose of20 lgÆkg )1 of morph<strong>in</strong>e compared with <strong>in</strong>travenoustechniques (323,324), <strong>and</strong> no difference <strong>in</strong> level ofsedation, nausea <strong>and</strong> vomit<strong>in</strong>g or pruritus (324). However,<strong>in</strong>trathecal morph<strong>in</strong>e <strong>in</strong> excess of 20 lgÆkg )1 wasassociated with respiratory depression (326). IT opiatesdid not affect the ability to monitor sp<strong>in</strong>al sensoryevoked potentials (SSEPs) (335).A meta-analysis of epidural analgesia <strong>in</strong> adolescentscoliosis surgery demonstrated a statistical, but cl<strong>in</strong>icallymodest improvement <strong>in</strong> pa<strong>in</strong> scores <strong>in</strong> patients receiv<strong>in</strong>gepidural analgesia compared with <strong>in</strong>travenous opioidson all first three postoperative days. One hundred <strong>and</strong>twenty patients from four studies were <strong>in</strong>cluded <strong>in</strong> theanalysis which also concluded that patient satisfactionwas higher <strong>in</strong> the epidural group. The papers <strong>in</strong>cluded <strong>in</strong>the meta-analysis differ <strong>in</strong> the regimens used: two papersreport the use of a s<strong>in</strong>gle catheter midthoracic epidural<strong>in</strong>fusion of bupivaca<strong>in</strong>e <strong>and</strong> fentanyl <strong>and</strong> show no difference<strong>in</strong> pa<strong>in</strong> sores compared PCA morph<strong>in</strong>e(330,331). The rema<strong>in</strong><strong>in</strong>g two papers report the use of adual catheter technique <strong>in</strong>fus<strong>in</strong>g ropivaca<strong>in</strong>e withoutopiod <strong>in</strong> patients follow<strong>in</strong>g posterior (329) <strong>and</strong> anterior(319) sp<strong>in</strong>al surgery. Significantly lower pa<strong>in</strong> scores wererecorded compared with cont<strong>in</strong>uous IV morph<strong>in</strong>e <strong>in</strong>fusion.A prospective comparison between PCEA with bipvaca<strong>in</strong>e0.1% <strong>and</strong> hydromorphone 10 lg/ml )1 <strong>and</strong>PCA hydromorphone demonstrated a reduction <strong>in</strong> pa<strong>in</strong>scores <strong>in</strong> the epidural group. There have also been severalretrospective series demonstrat<strong>in</strong>g reduced pa<strong>in</strong>scores with epidural analgesia compared with IV opioid:A s<strong>in</strong>gle epidural catheter <strong>in</strong>fus<strong>in</strong>g bupivaca<strong>in</strong>e withhydromorphone compared with a group receiv<strong>in</strong>g PCAmorph<strong>in</strong>e (613 patients); the epidural group had ahigher <strong>in</strong>cidence of side effects (333). Dual epiduralcatheters <strong>in</strong>fus<strong>in</strong>g 0.1% bupivaca<strong>in</strong>e with fentanyl2 lgÆml )1 compared with an opioid PCA, no difference<strong>in</strong> adverse effects (322). S<strong>in</strong>gle epidural <strong>in</strong>fus<strong>in</strong>g bupivaca<strong>in</strong>e0.1% <strong>and</strong> hydromorphone compared with PCAmorph<strong>in</strong>e compared with <strong>in</strong>trathecal <strong>and</strong> PCA morph<strong>in</strong>e:<strong>in</strong>trathecal morph<strong>in</strong>e controlled pa<strong>in</strong> equally asª 2012 Blackwell Publish<strong>in</strong>g Ltd, Pediatric Anesthesia, 22 (Suppl. 1), 1–79 51
- Page 1 and 2: PediatricAnesthesiaVolume 22 Supple
- Page 3 and 4: doi: 10.1111/j.1460-9592.2012.3838.
- Page 5 and 6: 1.6 Contact informationCorresponden
- Page 7 and 8: RecommendationsChildren’s self-re
- Page 9 and 10: Topical anesthetic preparations, fo
- Page 11 and 12: 2.7.6 Laparoscopic surgeryGood prac
- Page 13 and 14: In order to assess pain, effective
- Page 16 and 17: Postoperative painl NCCPC-PV (Non-C
- Page 18 and 19: 68 Broome ME, Richtsmeier A, Maikle
- Page 20 and 21: however, reductions in the response
- Page 22 and 23: increased success rate (i.e., less
- Page 24 and 25: Newer preparations such as liposoma
- Page 26 and 27: Good practice pointLubricant contai
- Page 28 and 29: most effective. There are a number
- Page 30 and 31: 12 Bellieni C, Bagnoli F, Perrone S
- Page 32 and 33: venipuncture pain in a pediatric em
- Page 34 and 35: 172 van Twillert B, Bremer M, Faber
- Page 36 and 37: necessary to ensure that the patien
- Page 38 and 39: when compared with LA alone and sal
- Page 40 and 41: Peribulbar block improves early ana
- Page 42 and 43: Analgesia Table 5.5.1 Sub-umbilical
- Page 44 and 45: was more effective with less motor
- Page 46 and 47: with using landmark techniques (205
- Page 48 and 49: Good practice pointWound infiltrati
- Page 50 and 51: Analgesia Table 5.6.4 Urological Su
- Page 54 and 55: well as the epidural technique for
- Page 56 and 57: Good practice pointA multi-modal an
- Page 58 and 59: 14 Grainger J, Saravanappa N. Local
- Page 60 and 61: day-stay unit. Int J Paediatr Dent
- Page 62 and 63: tinuous epidural infusion in childr
- Page 64 and 65: 245 Morton NS, O’Brien K. Analges
- Page 66 and 67: 321 Taenzer AH, Clark C, Taenzer AH
- Page 68 and 69: Section 6.0AnalgesiaContents6.1 Ana
- Page 70 and 71: enhance systemic absorption. Lidoca
- Page 73 and 74: undergoes hepatic biotransformation
- Page 75 and 76: tein binding are reduced and the ha
- Page 77 and 78: a low-dose infusion but the child m
- Page 79 and 80: Table 6.6.1 Paracetamol dosing guid
- Page 81: steps that health care professional