Good Practice in Postoperative and Procedural Pain Management ...
Good Practice in Postoperative and Procedural Pain Management ...
Good Practice in Postoperative and Procedural Pain Management ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
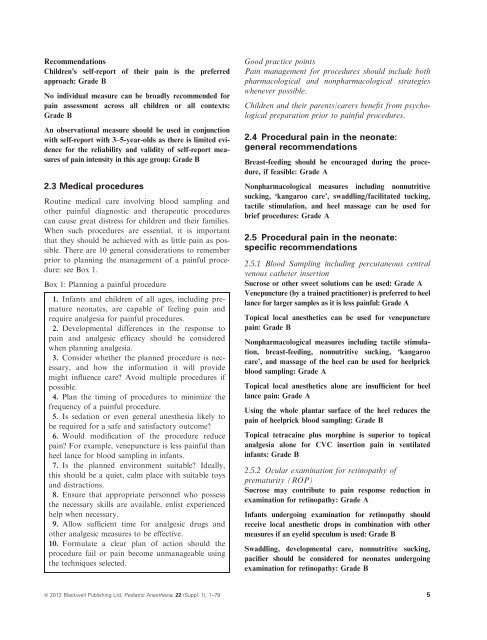
RecommendationsChildren’s self-report of their pa<strong>in</strong> is the preferredapproach: Grade BNo <strong>in</strong>dividual measure can be broadly recommended forpa<strong>in</strong> assessment across all children or all contexts:Grade BAn observational measure should be used <strong>in</strong> conjunctionwith self-report with 3–5-year-olds as there is limited evidencefor the reliability <strong>and</strong> validity of self-report measuresof pa<strong>in</strong> <strong>in</strong>tensity <strong>in</strong> this age group: Grade B2.3 Medical proceduresRout<strong>in</strong>e medical care <strong>in</strong>volv<strong>in</strong>g blood sampl<strong>in</strong>g <strong>and</strong>other pa<strong>in</strong>ful diagnostic <strong>and</strong> therapeutic procedurescan cause great distress for children <strong>and</strong> their families.When such procedures are essential, it is importantthat they should be achieved with as little pa<strong>in</strong> as possible.There are 10 general considerations to rememberprior to plann<strong>in</strong>g the management of a pa<strong>in</strong>ful procedure:see Box 1.Box 1: Plann<strong>in</strong>g a pa<strong>in</strong>ful procedure1. Infants <strong>and</strong> children of all ages, <strong>in</strong>clud<strong>in</strong>g prematureneonates, are capable of feel<strong>in</strong>g pa<strong>in</strong> <strong>and</strong>require analgesia for pa<strong>in</strong>ful procedures.2. Developmental differences <strong>in</strong> the response topa<strong>in</strong> <strong>and</strong> analgesic efficacy should be consideredwhen plann<strong>in</strong>g analgesia.3. Consider whether the planned procedure is necessary,<strong>and</strong> how the <strong>in</strong>formation it will providemight <strong>in</strong>fluence care? Avoid multiple procedures ifpossible.4. Plan the tim<strong>in</strong>g of procedures to m<strong>in</strong>imize thefrequency of a pa<strong>in</strong>ful procedure.5. Is sedation or even general anesthesia likely tobe required for a safe <strong>and</strong> satisfactory outcome?6. Would modification of the procedure reducepa<strong>in</strong>? For example, venepuncture is less pa<strong>in</strong>ful thanheel lance for blood sampl<strong>in</strong>g <strong>in</strong> <strong>in</strong>fants.7. Is the planned environment suitable? Ideally,this should be a quiet, calm place with suitable toys<strong>and</strong> distractions.8. Ensure that appropriate personnel who possessthe necessary skills are available, enlist experiencedhelp when necessary.9. Allow sufficient time for analgesic drugs <strong>and</strong>other analgesic measures to be effective.10. Formulate a clear plan of action should theprocedure fail or pa<strong>in</strong> become unmanageable us<strong>in</strong>gthe techniques selected.<strong>Good</strong> practice po<strong>in</strong>tsPa<strong>in</strong> management for procedures should <strong>in</strong>clude bothpharmacological <strong>and</strong> nonpharmacological strategieswhenever possible.Children <strong>and</strong> their parents/carers benefit from psychologicalpreparation prior to pa<strong>in</strong>ful procedures.2.4 <strong>Procedural</strong> pa<strong>in</strong> <strong>in</strong> the neonate:general recommendationsBreast-feed<strong>in</strong>g should be encouraged dur<strong>in</strong>g the procedure,if feasible: Grade ANonpharmacological measures <strong>in</strong>clud<strong>in</strong>g nonnutritivesuck<strong>in</strong>g, ‘kangaroo care’, swaddl<strong>in</strong>g/facilitated tuck<strong>in</strong>g,tactile stimulation, <strong>and</strong> heel massage can be used forbrief procedures: Grade A2.5 <strong>Procedural</strong> pa<strong>in</strong> <strong>in</strong> the neonate:specific recommendations2.5.1 Blood Sampl<strong>in</strong>g <strong>in</strong>clud<strong>in</strong>g percutaneous centralvenous catheter <strong>in</strong>sertionSucrose or other sweet solutions can be used: Grade AVenepuncture (by a tra<strong>in</strong>ed practitioner) is preferred to heellance for larger samples as it is less pa<strong>in</strong>ful: Grade ATopical local anesthetics can be used for venepuncturepa<strong>in</strong>: Grade BNonpharmacological measures <strong>in</strong>clud<strong>in</strong>g tactile stimulation,breast-feed<strong>in</strong>g, nonnutritive suck<strong>in</strong>g, ‘kangaroocare’, <strong>and</strong> massage of the heel can be used for heelprickblood sampl<strong>in</strong>g: Grade ATopical local anesthetics alone are <strong>in</strong>sufficient for heellance pa<strong>in</strong>: Grade AUs<strong>in</strong>g the whole plantar surface of the heel reduces thepa<strong>in</strong> of heelprick blood sampl<strong>in</strong>g: Grade BTopical tetraca<strong>in</strong>e plus morph<strong>in</strong>e is superior to topicalanalgesia alone for CVC <strong>in</strong>sertion pa<strong>in</strong> <strong>in</strong> ventilated<strong>in</strong>fants: Grade B2.5.2 Ocular exam<strong>in</strong>ation for ret<strong>in</strong>opathy ofprematurity (ROP)Sucrose may contribute to pa<strong>in</strong> response reduction <strong>in</strong>exam<strong>in</strong>ation for ret<strong>in</strong>opathy: Grade AInfants undergo<strong>in</strong>g exam<strong>in</strong>ation for ret<strong>in</strong>opathy shouldreceive local anesthetic drops <strong>in</strong> comb<strong>in</strong>ation with othermeasures if an eyelid speculum is used: Grade BSwaddl<strong>in</strong>g, developmental care, nonnutritive suck<strong>in</strong>g,pacifier should be considered for neonates undergo<strong>in</strong>gexam<strong>in</strong>ation for ret<strong>in</strong>opathy: Grade Bª 2012 Blackwell Publish<strong>in</strong>g Ltd, Pediatric Anesthesia, 22 (Suppl. 1), 1–79 5