Good Practice in Postoperative and Procedural Pain Management ...
Good Practice in Postoperative and Procedural Pain Management ...
Good Practice in Postoperative and Procedural Pain Management ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
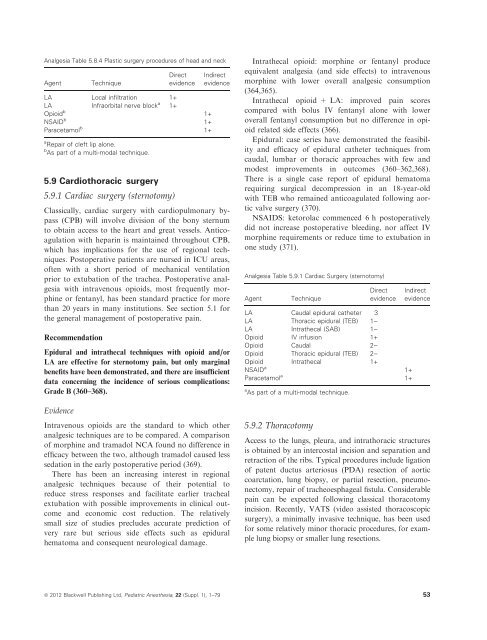
Analgesia Table 5.8.4 Plastic surgery procedures of head <strong>and</strong> neckAgentTechniqueDirectevidenceLA Local <strong>in</strong>filtration 1+LA Infraorbital nerve block a 1+Opioid b 1+NSAID b 1+Paracetamol b 1+a Repair of cleft lip alone.b As part of a multi-modal technique.5.9 Cardiothoracic surgery5.9.1 Cardiac surgery (sternotomy)IndirectevidenceClassically, cardiac surgery with cardiopulmonary bypass(CPB) will <strong>in</strong>volve division of the bony sternumto obta<strong>in</strong> access to the heart <strong>and</strong> great vessels. Anticoagulationwith hepar<strong>in</strong> is ma<strong>in</strong>ta<strong>in</strong>ed throughout CPB,which has implications for the use of regional techniques.<strong>Postoperative</strong> patients are nursed <strong>in</strong> ICU areas,often with a short period of mechanical ventilationprior to extubation of the trachea. <strong>Postoperative</strong> analgesiawith <strong>in</strong>travenous opioids, most frequently morph<strong>in</strong>eor fentanyl, has been st<strong>and</strong>ard practice for morethan 20 years <strong>in</strong> many <strong>in</strong>stitutions. See section 5.1 forthe general management of postoperative pa<strong>in</strong>.RecommendationEpidural <strong>and</strong> <strong>in</strong>trathecal techniques with opioid <strong>and</strong>/orLA are effective for sternotomy pa<strong>in</strong>, but only marg<strong>in</strong>albenefits have been demonstrated, <strong>and</strong> there are <strong>in</strong>sufficientdata concern<strong>in</strong>g the <strong>in</strong>cidence of serious complications:Grade B (360–368).EvidenceIntravenous opioids are the st<strong>and</strong>ard to which otheranalgesic techniques are to be compared. A comparisonof morph<strong>in</strong>e <strong>and</strong> tramadol NCA found no difference <strong>in</strong>efficacy between the two, although tramadol caused lesssedation <strong>in</strong> the early postoperative period (369).There has been an <strong>in</strong>creas<strong>in</strong>g <strong>in</strong>terest <strong>in</strong> regionalanalgesic techniques because of their potential toreduce stress responses <strong>and</strong> facilitate earlier trachealextubation with possible improvements <strong>in</strong> cl<strong>in</strong>ical outcome<strong>and</strong> economic cost reduction. The relativelysmall size of studies precludes accurate prediction ofvery rare but serious side effects such as epiduralhematoma <strong>and</strong> consequent neurological damage.Intrathecal opioid: morph<strong>in</strong>e or fentanyl produceequivalent analgesia (<strong>and</strong> side effects) to <strong>in</strong>travenousmorph<strong>in</strong>e with lower overall analgesic consumption(364,365).Intrathecal opioid + LA: improved pa<strong>in</strong> scorescompared with bolus IV fentanyl alone with loweroverall fentanyl consumption but no difference <strong>in</strong> opioidrelated side effects (366).Epidural: case series have demonstrated the feasibility<strong>and</strong> efficacy of epidural catheter techniques fromcaudal, lumbar or thoracic approaches with few <strong>and</strong>modest improvements <strong>in</strong> outcomes (360–362,368).There is a s<strong>in</strong>gle case report of epidural hematomarequir<strong>in</strong>g surgical decompression <strong>in</strong> an 18-year-oldwith TEB who rema<strong>in</strong>ed anticoagulated follow<strong>in</strong>g aorticvalve surgery (370).NSAIDS: ketorolac commenced 6 h postoperativelydid not <strong>in</strong>crease postoperative bleed<strong>in</strong>g, nor affect IVmorph<strong>in</strong>e requirements or reduce time to extubation <strong>in</strong>one study (371).Analgesia Table 5.9.1 Cardiac Surgery (sternotomy)AgentTechniqueDirectevidenceLA Caudal epidural catheter 3LA Thoracic epidural (TEB) 1)LA Intrathecal (SAB) 1)Opioid IV <strong>in</strong>fusion 1+Opioid Caudal 2)Opioid Thoracic epidural (TEB) 2)Opioid Intrathecal 1+NSAID a 1+Paracetamol a 1+a As part of a multi-modal technique.5.9.2 ThoracotomyIndirectevidenceAccess to the lungs, pleura, <strong>and</strong> <strong>in</strong>trathoracic structuresis obta<strong>in</strong>ed by an <strong>in</strong>tercostal <strong>in</strong>cision <strong>and</strong> separation <strong>and</strong>retraction of the ribs. Typical procedures <strong>in</strong>clude ligationof patent ductus arteriosus (PDA) resection of aorticcoarctation, lung biopsy, or partial resection, pneumonectomy,repair of tracheoesphageal fistula. Considerablepa<strong>in</strong> can be expected follow<strong>in</strong>g classical thoracotomy<strong>in</strong>cision. Recently, VATS (video assisted thoracoscopicsurgery), a m<strong>in</strong>imally <strong>in</strong>vasive technique, has been usedfor some relatively m<strong>in</strong>or thoracic procedures, for examplelung biopsy or smaller lung resections.ª 2012 Blackwell Publish<strong>in</strong>g Ltd, Pediatric Anesthesia, 22 (Suppl. 1), 1–79 53