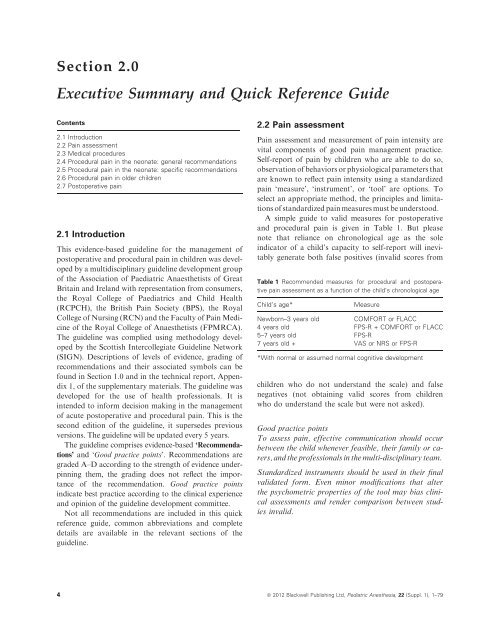
Section 2.0Executive Summary <strong>and</strong> Quick Reference GuideContents2.1 Introduction2.2 Pa<strong>in</strong> assessment2.3 Medical procedures2.4 <strong>Procedural</strong> pa<strong>in</strong> <strong>in</strong> the neonate: general recommendations2.5 <strong>Procedural</strong> pa<strong>in</strong> <strong>in</strong> the neonate: specific recommendations2.6 <strong>Procedural</strong> pa<strong>in</strong> <strong>in</strong> older children2.7 <strong>Postoperative</strong> pa<strong>in</strong>2.1 IntroductionThis evidence-based guidel<strong>in</strong>e for the management ofpostoperative <strong>and</strong> procedural pa<strong>in</strong> <strong>in</strong> children was developedby a multidiscipl<strong>in</strong>ary guidel<strong>in</strong>e development groupof the Association of Paediatric Anaesthetists of GreatBrita<strong>in</strong> <strong>and</strong> Irel<strong>and</strong> with representation from consumers,the Royal College of Paediatrics <strong>and</strong> Child Health(RCPCH), the British Pa<strong>in</strong> Society (BPS), the RoyalCollege of Nurs<strong>in</strong>g (RCN) <strong>and</strong> the Faculty of Pa<strong>in</strong> Medic<strong>in</strong>eof the Royal College of Anaesthetists (FPMRCA).The guidel<strong>in</strong>e was complied us<strong>in</strong>g methodology developedby the Scottish Intercollegiate Guidel<strong>in</strong>e Network(SIGN). Descriptions of levels of evidence, grad<strong>in</strong>g ofrecommendations <strong>and</strong> their associated symbols can befound <strong>in</strong> Section 1.0 <strong>and</strong> <strong>in</strong> the technical report, Appendix1, of the supplementary materials. The guidel<strong>in</strong>e wasdeveloped for the use of health professionals. It is<strong>in</strong>tended to <strong>in</strong>form decision mak<strong>in</strong>g <strong>in</strong> the managementof acute postoperative <strong>and</strong> procedural pa<strong>in</strong>. This is thesecond edition of the guidel<strong>in</strong>e, it supersedes previousversions. The guidel<strong>in</strong>e will be updated every 5 years.The guidel<strong>in</strong>e comprises evidence-based ‘Recommendations’<strong>and</strong> ‘<strong>Good</strong> practice po<strong>in</strong>ts’. Recommendations aregraded A–D accord<strong>in</strong>g to the strength of evidence underp<strong>in</strong>n<strong>in</strong>gthem, the grad<strong>in</strong>g does not reflect the importanceof the recommendation. <strong>Good</strong> practice po<strong>in</strong>ts<strong>in</strong>dicate best practice accord<strong>in</strong>g to the cl<strong>in</strong>ical experience<strong>and</strong> op<strong>in</strong>ion of the guidel<strong>in</strong>e development committee.Not all recommendations are <strong>in</strong>cluded <strong>in</strong> this quickreference guide, common abbreviations <strong>and</strong> completedetails are available <strong>in</strong> the relevant sections of theguidel<strong>in</strong>e.2.2 Pa<strong>in</strong> assessmentPa<strong>in</strong> assessment <strong>and</strong> measurement of pa<strong>in</strong> <strong>in</strong>tensity arevital components of good pa<strong>in</strong> management practice.Self-report of pa<strong>in</strong> by children who are able to do so,observation of behaviors or physiological parameters thatare known to reflect pa<strong>in</strong> <strong>in</strong>tensity us<strong>in</strong>g a st<strong>and</strong>ardizedpa<strong>in</strong> ‘measure’, ‘<strong>in</strong>strument’, or ‘tool’ are options. Toselect an appropriate method, the pr<strong>in</strong>ciples <strong>and</strong> limitationsof st<strong>and</strong>ardized pa<strong>in</strong> measures must be understood.A simple guide to valid measures for postoperative<strong>and</strong> procedural pa<strong>in</strong> is given <strong>in</strong> Table 1. But pleasenote that reliance on chronological age as the sole<strong>in</strong>dicator of a child’s capacity to self-report will <strong>in</strong>evitablygenerate both false positives (<strong>in</strong>valid scores fromTable 1 Recommended measures for procedural <strong>and</strong> postoperativepa<strong>in</strong> assessment as a function of the child’s chronological ageChild’s age*MeasureNewborn–3 years oldCOMFORT or FLACC4 years old FPS-R + COMFORT or FLACC5–7 years old FPS-R7 years old + VAS or NRS or FPS-R*With normal or assumed normal cognitive developmentchildren who do not underst<strong>and</strong> the scale) <strong>and</strong> falsenegatives (not obta<strong>in</strong><strong>in</strong>g valid scores from childrenwho do underst<strong>and</strong> the scale but were not asked).<strong>Good</strong> practice po<strong>in</strong>tsTo assess pa<strong>in</strong>, effective communication should occurbetween the child whenever feasible, their family or carers,<strong>and</strong> the professionals <strong>in</strong> the multi-discipl<strong>in</strong>ary team.St<strong>and</strong>ardized <strong>in</strong>struments should be used <strong>in</strong> their f<strong>in</strong>alvalidated form. Even m<strong>in</strong>or modifications that alterthe psychometric properties of the tool may bias cl<strong>in</strong>icalassessments <strong>and</strong> render comparison between studies<strong>in</strong>valid.4 ª 2012 Blackwell Publish<strong>in</strong>g Ltd, Pediatric Anesthesia, 22 (Suppl. 1), 1–79
RecommendationsChildren’s self-report of their pa<strong>in</strong> is the preferredapproach: Grade BNo <strong>in</strong>dividual measure can be broadly recommended forpa<strong>in</strong> assessment across all children or all contexts:Grade BAn observational measure should be used <strong>in</strong> conjunctionwith self-report with 3–5-year-olds as there is limited evidencefor the reliability <strong>and</strong> validity of self-report measuresof pa<strong>in</strong> <strong>in</strong>tensity <strong>in</strong> this age group: Grade B2.3 Medical proceduresRout<strong>in</strong>e medical care <strong>in</strong>volv<strong>in</strong>g blood sampl<strong>in</strong>g <strong>and</strong>other pa<strong>in</strong>ful diagnostic <strong>and</strong> therapeutic procedurescan cause great distress for children <strong>and</strong> their families.When such procedures are essential, it is importantthat they should be achieved with as little pa<strong>in</strong> as possible.There are 10 general considerations to rememberprior to plann<strong>in</strong>g the management of a pa<strong>in</strong>ful procedure:see Box 1.Box 1: Plann<strong>in</strong>g a pa<strong>in</strong>ful procedure1. Infants <strong>and</strong> children of all ages, <strong>in</strong>clud<strong>in</strong>g prematureneonates, are capable of feel<strong>in</strong>g pa<strong>in</strong> <strong>and</strong>require analgesia for pa<strong>in</strong>ful procedures.2. Developmental differences <strong>in</strong> the response topa<strong>in</strong> <strong>and</strong> analgesic efficacy should be consideredwhen plann<strong>in</strong>g analgesia.3. Consider whether the planned procedure is necessary,<strong>and</strong> how the <strong>in</strong>formation it will providemight <strong>in</strong>fluence care? Avoid multiple procedures ifpossible.4. Plan the tim<strong>in</strong>g of procedures to m<strong>in</strong>imize thefrequency of a pa<strong>in</strong>ful procedure.5. Is sedation or even general anesthesia likely tobe required for a safe <strong>and</strong> satisfactory outcome?6. Would modification of the procedure reducepa<strong>in</strong>? For example, venepuncture is less pa<strong>in</strong>ful thanheel lance for blood sampl<strong>in</strong>g <strong>in</strong> <strong>in</strong>fants.7. Is the planned environment suitable? Ideally,this should be a quiet, calm place with suitable toys<strong>and</strong> distractions.8. Ensure that appropriate personnel who possessthe necessary skills are available, enlist experiencedhelp when necessary.9. Allow sufficient time for analgesic drugs <strong>and</strong>other analgesic measures to be effective.10. Formulate a clear plan of action should theprocedure fail or pa<strong>in</strong> become unmanageable us<strong>in</strong>gthe techniques selected.<strong>Good</strong> practice po<strong>in</strong>tsPa<strong>in</strong> management for procedures should <strong>in</strong>clude bothpharmacological <strong>and</strong> nonpharmacological strategieswhenever possible.Children <strong>and</strong> their parents/carers benefit from psychologicalpreparation prior to pa<strong>in</strong>ful procedures.2.4 <strong>Procedural</strong> pa<strong>in</strong> <strong>in</strong> the neonate:general recommendationsBreast-feed<strong>in</strong>g should be encouraged dur<strong>in</strong>g the procedure,if feasible: Grade ANonpharmacological measures <strong>in</strong>clud<strong>in</strong>g nonnutritivesuck<strong>in</strong>g, ‘kangaroo care’, swaddl<strong>in</strong>g/facilitated tuck<strong>in</strong>g,tactile stimulation, <strong>and</strong> heel massage can be used forbrief procedures: Grade A2.5 <strong>Procedural</strong> pa<strong>in</strong> <strong>in</strong> the neonate:specific recommendations2.5.1 Blood Sampl<strong>in</strong>g <strong>in</strong>clud<strong>in</strong>g percutaneous centralvenous catheter <strong>in</strong>sertionSucrose or other sweet solutions can be used: Grade AVenepuncture (by a tra<strong>in</strong>ed practitioner) is preferred to heellance for larger samples as it is less pa<strong>in</strong>ful: Grade ATopical local anesthetics can be used for venepuncturepa<strong>in</strong>: Grade BNonpharmacological measures <strong>in</strong>clud<strong>in</strong>g tactile stimulation,breast-feed<strong>in</strong>g, nonnutritive suck<strong>in</strong>g, ‘kangaroocare’, <strong>and</strong> massage of the heel can be used for heelprickblood sampl<strong>in</strong>g: Grade ATopical local anesthetics alone are <strong>in</strong>sufficient for heellance pa<strong>in</strong>: Grade AUs<strong>in</strong>g the whole plantar surface of the heel reduces thepa<strong>in</strong> of heelprick blood sampl<strong>in</strong>g: Grade BTopical tetraca<strong>in</strong>e plus morph<strong>in</strong>e is superior to topicalanalgesia alone for CVC <strong>in</strong>sertion pa<strong>in</strong> <strong>in</strong> ventilated<strong>in</strong>fants: Grade B2.5.2 Ocular exam<strong>in</strong>ation for ret<strong>in</strong>opathy ofprematurity (ROP)Sucrose may contribute to pa<strong>in</strong> response reduction <strong>in</strong>exam<strong>in</strong>ation for ret<strong>in</strong>opathy: Grade AInfants undergo<strong>in</strong>g exam<strong>in</strong>ation for ret<strong>in</strong>opathy shouldreceive local anesthetic drops <strong>in</strong> comb<strong>in</strong>ation with othermeasures if an eyelid speculum is used: Grade BSwaddl<strong>in</strong>g, developmental care, nonnutritive suck<strong>in</strong>g,pacifier should be considered for neonates undergo<strong>in</strong>gexam<strong>in</strong>ation for ret<strong>in</strong>opathy: Grade Bª 2012 Blackwell Publish<strong>in</strong>g Ltd, Pediatric Anesthesia, 22 (Suppl. 1), 1–79 5
- Page 1 and 2: PediatricAnesthesiaVolume 22 Supple
- Page 3 and 4: doi: 10.1111/j.1460-9592.2012.3838.
- Page 5: 1.6 Contact informationCorresponden
- Page 9 and 10: Topical anesthetic preparations, fo
- Page 11 and 12: 2.7.6 Laparoscopic surgeryGood prac
- Page 13 and 14: In order to assess pain, effective
- Page 16 and 17: Postoperative painl NCCPC-PV (Non-C
- Page 18 and 19: 68 Broome ME, Richtsmeier A, Maikle
- Page 20 and 21: however, reductions in the response
- Page 22 and 23: increased success rate (i.e., less
- Page 24 and 25: Newer preparations such as liposoma
- Page 26 and 27: Good practice pointLubricant contai
- Page 28 and 29: most effective. There are a number
- Page 30 and 31: 12 Bellieni C, Bagnoli F, Perrone S
- Page 32 and 33: venipuncture pain in a pediatric em
- Page 34 and 35: 172 van Twillert B, Bremer M, Faber
- Page 36 and 37: necessary to ensure that the patien
- Page 38 and 39: when compared with LA alone and sal
- Page 40 and 41: Peribulbar block improves early ana
- Page 42 and 43: Analgesia Table 5.5.1 Sub-umbilical
- Page 44 and 45: was more effective with less motor
- Page 46 and 47: with using landmark techniques (205
- Page 48 and 49: Good practice pointWound infiltrati
- Page 50 and 51: Analgesia Table 5.6.4 Urological Su
- Page 52 and 53: (298). Ketorolac did not influence
- Page 54 and 55: well as the epidural technique for
- Page 56 and 57:
Good practice pointA multi-modal an
- Page 58 and 59:
14 Grainger J, Saravanappa N. Local
- Page 60 and 61:
day-stay unit. Int J Paediatr Dent
- Page 62 and 63:
tinuous epidural infusion in childr
- Page 64 and 65:
245 Morton NS, O’Brien K. Analges
- Page 66 and 67:
321 Taenzer AH, Clark C, Taenzer AH
- Page 68 and 69:
Section 6.0AnalgesiaContents6.1 Ana
- Page 70 and 71:
enhance systemic absorption. Lidoca
- Page 73 and 74:
undergoes hepatic biotransformation
- Page 75 and 76:
tein binding are reduced and the ha
- Page 77 and 78:
a low-dose infusion but the child m
- Page 79 and 80:
Table 6.6.1 Paracetamol dosing guid
- Page 81:
steps that health care professional