Internal-Medicine
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
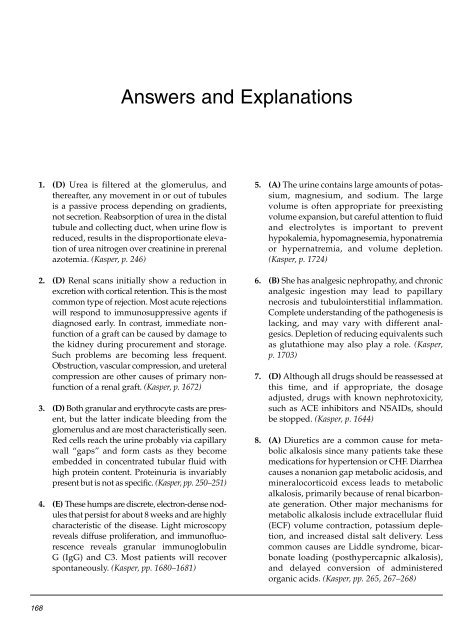
Answers and Explanations<br />
1. (D) Urea is filtered at the glomerulus, and<br />
thereafter, any movement in or out of tubules<br />
is a passive process depending on gradients,<br />
not secretion. Reabsorption of urea in the distal<br />
tubule and collecting duct, when urine flow is<br />
reduced, results in the disproportionate elevation<br />
of urea nitrogen over creatinine in prerenal<br />
azotemia. (Kasper, p. 246)<br />
2. (D) Renal scans initially show a reduction in<br />
excretion with cortical retention. This is the most<br />
common type of rejection. Most acute rejections<br />
will respond to immunosuppressive agents if<br />
diagnosed early. In contrast, immediate nonfunction<br />
of a graft can be caused by damage to<br />
the kidney during procurement and storage.<br />
Such problems are becoming less frequent.<br />
Obstruction, vascular compression, and ureteral<br />
compression are other causes of primary nonfunction<br />
of a renal graft. (Kasper, p. 1672)<br />
3. (D) Both granular and erythrocyte casts are present,<br />
but the latter indicate bleeding from the<br />
glomerulus and are most characteristically seen.<br />
Red cells reach the urine probably via capillary<br />
wall “gaps” and form casts as they become<br />
embedded in concentrated tubular fluid with<br />
high protein content. Proteinuria is invariably<br />
present but is not as specific. (Kasper, pp. 250–251)<br />
4. (E) These humps are discrete, electron-dense nodules<br />
that persist for about 8 weeks and are highly<br />
characteristic of the disease. Light microscopy<br />
reveals diffuse proliferation, and immunofluorescence<br />
reveals granular immunoglobulin<br />
G (IgG) and C3. Most patients will recover<br />
spontaneously. (Kasper, pp. 1680–1681)<br />
5. (A) The urine contains large amounts of potassium,<br />
magnesium, and sodium. The large<br />
volume is often appropriate for preexisting<br />
volume expansion, but careful attention to fluid<br />
and electrolytes is important to prevent<br />
hypokalemia, hypomagnesemia, hyponatremia<br />
or hypernatremia, and volume depletion.<br />
(Kasper, p. 1724)<br />
6. (B) She has analgesic nephropathy, and chronic<br />
analgesic ingestion may lead to papillary<br />
necrosis and tubulointerstitial inflammation.<br />
Complete understanding of the pathogenesis is<br />
lacking, and may vary with different analgesics.<br />
Depletion of reducing equivalents such<br />
as glutathione may also play a role. (Kasper,<br />
p. 1703)<br />
7. (D) Although all drugs should be reassessed at<br />
this time, and if appropriate, the dosage<br />
adjusted, drugs with known nephrotoxicity,<br />
such as ACE inhibitors and NSAIDs, should<br />
be stopped. (Kasper, p. 1644)<br />
8. (A) Diuretics are a common cause for metabolic<br />
alkalosis since many patients take these<br />
medications for hypertension or CHF. Diarrhea<br />
causes a nonanion gap metabolic acidosis, and<br />
mineralocorticoid excess leads to metabolic<br />
alkalosis, primarily because of renal bicarbonate<br />
generation. Other major mechanisms for<br />
metabolic alkalosis include extracellular fluid<br />
(ECF) volume contraction, potassium depletion,<br />
and increased distal salt delivery. Less<br />
common causes are Liddle syndrome, bicarbonate<br />
loading (posthypercapnic alkalosis),<br />
and delayed conversion of administered<br />
organic acids. (Kasper, pp. 265, 267–268)<br />
168