national-clinical-guidelines-for-stroke-fourth-edition
national-clinical-guidelines-for-stroke-fourth-edition
national-clinical-guidelines-for-stroke-fourth-edition
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
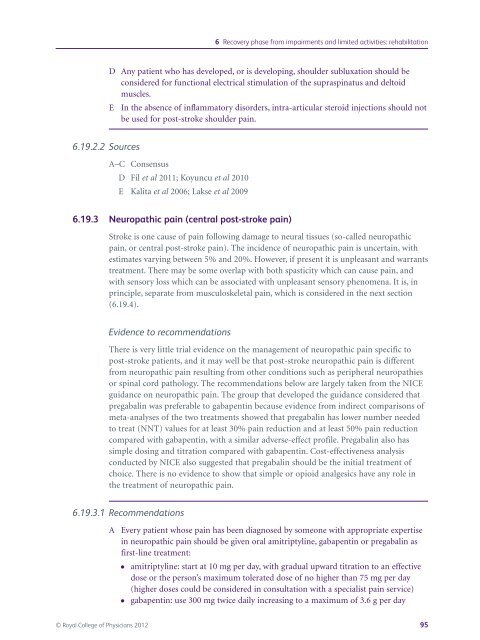
D Any patient who has developed, or is developing, shoulder subluxation should be<br />
considered <strong>for</strong> functional electrical stimulation of the supraspinatus and deltoid<br />
muscles.<br />
E In the absence of inflammatory disorders, intra-articular steroid injections should not<br />
be used <strong>for</strong> post-<strong>stroke</strong> shoulder pain.<br />
6.19.2.2 Sources<br />
A–C Consensus<br />
D Fil et al 2011; Koyuncu et al 2010<br />
E Kalita et al 2006; Lakse et al 2009<br />
6.19.3 Neuropathic pain (central post-<strong>stroke</strong> pain)<br />
Stroke is one cause of pain following damage to neural tissues (so-called neuropathic<br />
pain, or central post-<strong>stroke</strong> pain). The incidence of neuropathic pain is uncertain, with<br />
estimates varying between 5% and 20%. However, if present it is unpleasant and warrants<br />
treatment. There may be some overlap with both spasticity which can cause pain, and<br />
with sensory loss which can be associated with unpleasant sensory phenomena. It is, in<br />
principle, separate from musculoskeletal pain, which is considered in the next section<br />
(6.19.4).<br />
Evidence to recommendations<br />
There is very little trial evidence on the management of neuropathic pain specific to<br />
post-<strong>stroke</strong> patients, and it may well be that post-<strong>stroke</strong> neuropathic pain is different<br />
from neuropathic pain resulting from other conditions such as peripheral neuropathies<br />
or spinal cord pathology. The recommendations below are largely taken from the NICE<br />
guidance on neuropathic pain. The group that developed the guidance considered that<br />
pregabalin was preferable to gabapentin because evidence from indirect comparisons of<br />
meta-analyses of the two treatments showed that pregabalin has lower number needed<br />
to treat (NNT) values <strong>for</strong> at least 30% pain reduction and at least 50% pain reduction<br />
compared with gabapentin, with a similar adverse-effect profile. Pregabalin also has<br />
simple dosing and titration compared with gabapentin. Cost-effectiveness analysis<br />
conducted by NICE also suggested that pregabalin should be the initial treatment of<br />
choice. There is no evidence to show that simple or opioid analgesics have any role in<br />
the treatment of neuropathic pain.<br />
6.19.3.1 Recommendations<br />
6 Recovery phase from impairments and limited activities: rehabilitation<br />
A Every patient whose pain has been diagnosed by someone with appropriate expertise<br />
in neuropathic pain should be given oral amitriptyline, gabapentin or pregabalin as<br />
first-line treatment:<br />
● amitriptyline: start at 10 mg per day, with gradual upward titration to an effective<br />
dose or the person’s maximum tolerated dose of no higher than 75 mg per day<br />
(higher doses could be considered in consultation with a specialist pain service)<br />
● gabapentin: use 300 mg twice daily increasing to a maximum of 3.6 g per day<br />
© Royal College of Physicians 2012 95