national-clinical-guidelines-for-stroke-fourth-edition
national-clinical-guidelines-for-stroke-fourth-edition
national-clinical-guidelines-for-stroke-fourth-edition
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
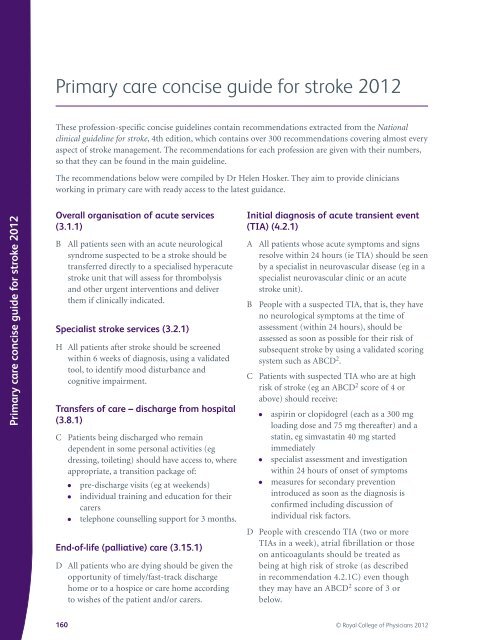
Primary care concise guide <strong>for</strong> <strong>stroke</strong> 2012<br />
Primary care concise guide <strong>for</strong> <strong>stroke</strong> 2012<br />
These profession-specific concise <strong>guidelines</strong> contain recommendations extracted from the National<br />
<strong>clinical</strong> guideline <strong>for</strong> <strong>stroke</strong>, 4th <strong>edition</strong>, which contains over 300 recommendations covering almost every<br />
aspect of <strong>stroke</strong> management. The recommendations <strong>for</strong> each profession are given with their numbers,<br />
so that they can be found in the main guideline.<br />
The recommendations below were compiled by Dr Helen Hosker. They aim to provide clinicians<br />
working in primary care with ready access to the latest guidance.<br />
Overall organisation of acute services<br />
(3.1.1)<br />
B All patients seen with an acute neurological<br />
syndrome suspected to be a <strong>stroke</strong> should be<br />
transferred directly to a specialised hyperacute<br />
<strong>stroke</strong> unit that will assess <strong>for</strong> thrombolysis<br />
and other urgent interventions and deliver<br />
them if <strong>clinical</strong>ly indicated.<br />
Specialist <strong>stroke</strong> services (3.2.1)<br />
H All patients after <strong>stroke</strong> should be screened<br />
within 6 weeks of diagnosis, using a validated<br />
tool, to identify mood disturbance and<br />
cognitive impairment.<br />
Transfers of care – discharge from hospital<br />
(3.8.1)<br />
C Patients being discharged who remain<br />
dependent in some personal activities (eg<br />
dressing, toileting) should have access to, where<br />
appropriate, a transition package of:<br />
● pre-discharge visits (eg at weekends)<br />
● individual training and education <strong>for</strong> their<br />
carers<br />
● telephone counselling support <strong>for</strong> 3 months.<br />
End-of-life (palliative) care (3.15.1)<br />
D All patients who are dying should be given the<br />
opportunity of timely/fast-track discharge<br />
home or to a hospice or care home according<br />
to wishes of the patient and/or carers.<br />
Initial diagnosis of acute transient event<br />
(TIA) (4.2.1)<br />
A All patients whose acute symptoms and signs<br />
resolve within 24 hours (ie TIA) should be seen<br />
by a specialist in neurovascular disease (eg in a<br />
specialist neurovascular clinic or an acute<br />
<strong>stroke</strong> unit).<br />
B People with a suspected TIA, that is, they have<br />
no neurological symptoms at the time of<br />
assessment (within 24 hours), should be<br />
assessed as soon as possible <strong>for</strong> their risk of<br />
subsequent <strong>stroke</strong> by using a validated scoring<br />
system such as ABCD 2 .<br />
C Patients with suspected TIA who are at high<br />
risk of <strong>stroke</strong> (eg an ABCD 2 score of 4 or<br />
above) should receive:<br />
● aspirin or clopidogrel (each as a 300 mg<br />
loading dose and 75 mg thereafter) and a<br />
statin, eg simvastatin 40 mg started<br />
immediately<br />
● specialist assessment and investigation<br />
within 24 hours of onset of symptoms<br />
● measures <strong>for</strong> secondary prevention<br />
introduced as soon as the diagnosis is<br />
confirmed including discussion of<br />
individual risk factors.<br />
D People with crescendo TIA (two or more<br />
TIAs in a week), atrial fibrillation or those<br />
on anticoagulants should be treated as<br />
being at high risk of <strong>stroke</strong> (as described<br />
in recommendation 4.2.1C) even though<br />
they may have an ABCD 2 score of 3 or<br />
below.<br />
160 © Royal College of Physicians 2012