national-clinical-guidelines-for-stroke-fourth-edition
national-clinical-guidelines-for-stroke-fourth-edition
national-clinical-guidelines-for-stroke-fourth-edition
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
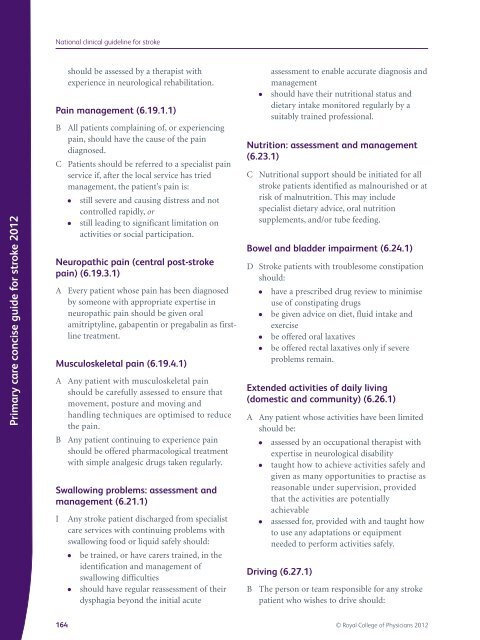
Primary care concise guide <strong>for</strong> <strong>stroke</strong> 2012<br />
National <strong>clinical</strong> guideline <strong>for</strong> <strong>stroke</strong><br />
should be assessed by a therapist with<br />
experience in neurological rehabilitation.<br />
Pain management (6.19.1.1)<br />
B All patients complaining of, or experiencing<br />
pain, should have the cause of the pain<br />
diagnosed.<br />
C Patients should be referred to a specialist pain<br />
service if, after the local service has tried<br />
management, the patient’s pain is:<br />
● still severe and causing distress and not<br />
controlled rapidly, or<br />
● still leading to significant limitation on<br />
activities or social participation.<br />
Neuropathic pain (central post-<strong>stroke</strong><br />
pain) (6.19.3.1)<br />
A Every patient whose pain has been diagnosed<br />
by someone with appropriate expertise in<br />
neuropathic pain should be given oral<br />
amitriptyline, gabapentin or pregabalin as firstline<br />
treatment.<br />
Musculoskeletal pain (6.19.4.1)<br />
A Any patient with musculoskeletal pain<br />
should be carefully assessed to ensure that<br />
movement, posture and moving and<br />
handling techniques are optimised to reduce<br />
the pain.<br />
B Any patient continuing to experience pain<br />
should be offered pharmacological treatment<br />
with simple analgesic drugs taken regularly.<br />
Swallowing problems: assessment and<br />
management (6.21.1)<br />
I Any <strong>stroke</strong> patient discharged from specialist<br />
care services with continuing problems with<br />
swallowing food or liquid safely should:<br />
● be trained, or have carers trained, in the<br />
identification and management of<br />
swallowing difficulties<br />
● should have regular reassessment of their<br />
dysphagia beyond the initial acute<br />
assessment to enable accurate diagnosis and<br />
management<br />
● should have their nutritional status and<br />
dietary intake monitored regularly by a<br />
suitably trained professional.<br />
Nutrition: assessment and management<br />
(6.23.1)<br />
C Nutritional support should be initiated <strong>for</strong> all<br />
<strong>stroke</strong> patients identified as malnourished or at<br />
risk of malnutrition. This may include<br />
specialist dietary advice, oral nutrition<br />
supplements, and/or tube feeding.<br />
Bowel and bladder impairment (6.24.1)<br />
D Stroke patients with troublesome constipation<br />
should:<br />
● have a prescribed drug review to minimise<br />
use of constipating drugs<br />
● be given advice on diet, fluid intake and<br />
exercise<br />
● be offered oral laxatives<br />
● be offered rectal laxatives only if severe<br />
problems remain.<br />
Extended activities of daily living<br />
(domestic and community) (6.26.1)<br />
A Any patient whose activities have been limited<br />
should be:<br />
● assessed by an occupational therapist with<br />
expertise in neurological disability<br />
● taught how to achieve activities safely and<br />
given as many opportunities to practise as<br />
reasonable under supervision, provided<br />
that the activities are potentially<br />
achievable<br />
● assessed <strong>for</strong>, provided with and taught how<br />
to use any adaptations or equipment<br />
needed to per<strong>for</strong>m activities safely.<br />
Driving (6.27.1)<br />
B The person or team responsible <strong>for</strong> any <strong>stroke</strong><br />
patient who wishes to drive should:<br />
164 © Royal College of Physicians 2012