Consultant physicians working with patients - Royal College of ...
Consultant physicians working with patients - Royal College of ...
Consultant physicians working with patients - Royal College of ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
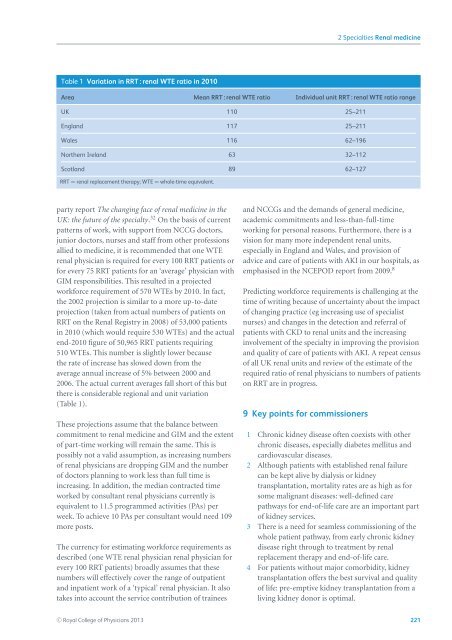
2 Specialties Renal medicineTable 1 Variation in RRT : renal WTE ratio in 2010Area Mean RRT : renal WTE ratio Individual unit RRT : renal WTE ratio rangeUK 110 25–211England 117 25–211Wales 116 62–196Northern Ireland 63 32–112Scotland 89 62–127RRT = renal replacement therapy; WTE = whole-time equivalent.party report The changing face <strong>of</strong> renal medicine in theUK: the future <strong>of</strong> the specialty. 32 On the basis <strong>of</strong> currentpatterns <strong>of</strong> work, <strong>with</strong> support from NCCG doctors,junior doctors, nurses and staff from other pr<strong>of</strong>essionsallied to medicine, it is recommended that one WTErenal physician is required for every 100 RRT <strong>patients</strong> orfor every 75 RRT <strong>patients</strong> for an ‘average’ physician <strong>with</strong>GIM responsibilities. This resulted in a projectedworkforce requirement <strong>of</strong> 570 WTEs by 2010. In fact,the 2002 projection is similar to a more up-to-dateprojection (taken from actual numbers <strong>of</strong> <strong>patients</strong> onRRT on the Renal Registry in 2008) <strong>of</strong> 53,000 <strong>patients</strong>in 2010 (which would require 530 WTEs) and the actualend-2010 figure <strong>of</strong> 50,965 RRT <strong>patients</strong> requiring510 WTEs. This number is slightly lower becausethe rate <strong>of</strong> increase has slowed down from theaverage annual increase <strong>of</strong> 5% between 2000 and2006. The actual current averages fall short <strong>of</strong> this butthere is considerable regional and unit variation(Table 1).These projections assume that the balance betweencommitment to renal medicine and GIM and the extent<strong>of</strong> part-time <strong>working</strong> will remain the same. This ispossibly not a valid assumption, as increasing numbers<strong>of</strong> renal <strong>physicians</strong> are dropping GIM and the number<strong>of</strong> doctors planning to work less than full time isincreasing. In addition, the median contracted timeworked by consultant renal <strong>physicians</strong> currently isequivalent to 11.5 programmed activities (PAs) perweek. To achieve 10 PAs per consultant would need 109more posts.The currency for estimating workforce requirements asdescribed (one WTE renal physician renal physician forevery 100 RRT <strong>patients</strong>) broadly assumes that thesenumbers will effectively cover the range <strong>of</strong> outpatientand inpatient work <strong>of</strong> a ‘typical’ renal physician. It alsotakes into account the service contribution <strong>of</strong> traineesand NCCGs and the demands <strong>of</strong> general medicine,academic commitments and less-than-full-time<strong>working</strong> for personal reasons. Furthermore, there is avision for many more independent renal units,especially in England and Wales, and provision <strong>of</strong>advice and care <strong>of</strong> <strong>patients</strong> <strong>with</strong> AKI in our hospitals, asemphasised in the NCEPOD report from 2009. 8Predicting workforce requirements is challenging at thetime <strong>of</strong> writing because <strong>of</strong> uncertainty about the impact<strong>of</strong> changing practice (eg increasing use <strong>of</strong> specialistnurses) and changes in the detection and referral <strong>of</strong><strong>patients</strong> <strong>with</strong> CKD to renal units and the increasinginvolvement <strong>of</strong> the specialty in improving the provisionand quality <strong>of</strong> care <strong>of</strong> <strong>patients</strong> <strong>with</strong> AKI. A repeat census<strong>of</strong> all UK renal units and review <strong>of</strong> the estimate <strong>of</strong> therequired ratio <strong>of</strong> renal <strong>physicians</strong> to numbers <strong>of</strong> <strong>patients</strong>on RRT are in progress.9 Key points for commissioners1 Chronic kidney disease <strong>of</strong>ten coexists <strong>with</strong> otherchronic diseases, especially diabetes mellitus andcardiovascular diseases.2 Although <strong>patients</strong> <strong>with</strong> established renal failurecan be kept alive by dialysis or kidneytransplantation, mortality rates are as high as forsome malignant diseases: well-defined carepathways for end-<strong>of</strong>-life care are an important part<strong>of</strong> kidney services.3 There is a need for seamless commissioning <strong>of</strong> thewhole patient pathway, from early chronic kidneydisease right through to treatment by renalreplacement therapy and end-<strong>of</strong>-life care.4 For <strong>patients</strong> <strong>with</strong>out major comorbidity, kidneytransplantation <strong>of</strong>fers the best survival and quality<strong>of</strong> life: pre-emptive kidney transplantation from aliving kidney donor is optimal.C○ <strong>Royal</strong> <strong>College</strong> <strong>of</strong> Physicians 2013 221