Consultant physicians working with patients - Royal College of ...
Consultant physicians working with patients - Royal College of ...
Consultant physicians working with patients - Royal College of ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
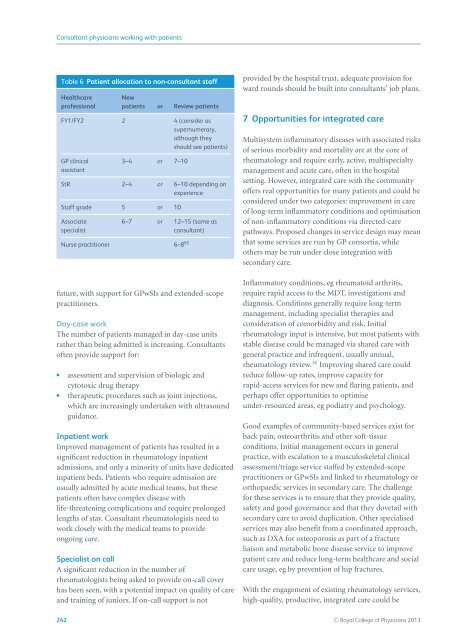
<strong>Consultant</strong> <strong>physicians</strong> <strong>working</strong> <strong>with</strong> <strong>patients</strong>Table 6 Patient allocation to non-consultant staffHealthcarepr<strong>of</strong>essionalNew<strong>patients</strong> or Review <strong>patients</strong>FY1/FY2 2 4 (consider assupernumerary,although theyshould see <strong>patients</strong>)GP clinicalassistant3–4 or 7–10StR 2–4 or 6–10 depending onexperienceStaff grade 5 or 10Associatespecialist6–7 or 12–15 (same asconsultant)Nurse practitioner 6–8 65future, <strong>with</strong> support for GPwSIs and extended-scopepractitioners.Day-case workThe number <strong>of</strong> <strong>patients</strong> managed in day-case unitsrather than being admitted is increasing. <strong>Consultant</strong>s<strong>of</strong>ten provide support for: assessment and supervision <strong>of</strong> biologic andcytotoxic drug therapy therapeutic procedures such as joint injections,which are increasingly undertaken <strong>with</strong> ultrasoundguidance.Inpatient workImproved management <strong>of</strong> <strong>patients</strong> has resulted in asignificant reduction in rheumatology inpatientadmissions, and only a minority <strong>of</strong> units have dedicatedinpatient beds. Patients who require admission areusually admitted by acute medical teams, but these<strong>patients</strong> <strong>of</strong>ten have complex disease <strong>with</strong>life-threatening complications and require prolongedlengths <strong>of</strong> stay. <strong>Consultant</strong> rheumatologists need towork closely <strong>with</strong> the medical teams to provideongoing care.Specialist on callA significant reduction in the number <strong>of</strong>rheumatologists being asked to provide on-call coverhas been seen, <strong>with</strong> a potential impact on quality <strong>of</strong> careand training <strong>of</strong> juniors. If on-call support is notprovided by the hospital trust, adequate provision forward rounds should be built into consultants’ job plans.7 Opportunities for integrated careMultisystem inflammatory diseases <strong>with</strong> associated risks<strong>of</strong> serious morbidity and mortality are at the core <strong>of</strong>rheumatology and require early, active, multispecialtymanagement and acute care, <strong>of</strong>ten in the hospitalsetting. However, integrated care <strong>with</strong> the community<strong>of</strong>fers real opportunities for many <strong>patients</strong> and could beconsidered under two categories: improvement in care<strong>of</strong> long-term inflammatory conditions and optimisation<strong>of</strong> non-inflammatory conditions via directed-carepathways. Proposed changes in service design may meanthat some services are run by GP consortia, whileothers may be run under close integration <strong>with</strong>secondary care.Inflammatory conditions, eg rheumatoid arthritis,require rapid access to the MDT, investigations anddiagnosis. Conditions generally require long-termmanagement, including specialist therapies andconsideration <strong>of</strong> comorbidity and risk. Initialrheumatology input is intensive, but most <strong>patients</strong> <strong>with</strong>stable disease could be managed via shared care <strong>with</strong>general practice and infrequent, usually annual,rheumatology review. 16 Improving shared care couldreduce follow-up rates, improve capacity forrapid-access services for new and flaring <strong>patients</strong>, andperhaps <strong>of</strong>fer opportunities to optimiseunder-resourced areas, eg podiatry and psychology.Good examples <strong>of</strong> community-based services exist forback pain, osteoarthritis and other s<strong>of</strong>t-tissueconditions. Initial management occurs in generalpractice, <strong>with</strong> escalation to a musculoskeletal clinicalassessment/triage service staffed by extended-scopepractitioners or GPwSIs and linked to rheumatology ororthopaedic services in secondary care. The challengefor these services is to ensure that they provide quality,safety and good governance and that they dovetail <strong>with</strong>secondary care to avoid duplication. Other specialisedservices may also benefit from a coordinated approach,such as DXA for osteoporosis as part <strong>of</strong> a fractureliaison and metabolic bone disease service to improvepatient care and reduce long-term healthcare and socialcare usage, eg by prevention <strong>of</strong> hip fractures.With the engagement <strong>of</strong> existing rheumatology services,high-quality, productive, integrated care could be242 C○ <strong>Royal</strong> <strong>College</strong> <strong>of</strong> Physicians 2013