Anorectal Manometry in 3D NEW! - Swiss-knife.org
Anorectal Manometry in 3D NEW! - Swiss-knife.org
Anorectal Manometry in 3D NEW! - Swiss-knife.org
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
normal angiogenesis <strong>in</strong>duced by cells produc<strong>in</strong>g high levels of hVEGF was not due to a rapid loss of<br />
expression <strong>in</strong> vivo.<br />
Conclusion: Human VEGF165 displayed a radically different dose-effect relationship compared to<br />
mur<strong>in</strong>e VEGF164 <strong>in</strong> a highly controlled <strong>in</strong> vivo model, <strong>in</strong>duc<strong>in</strong>g only normal angiogenesis despite much<br />
higher microenvironmental expression levels. These data suggest that the therapeutic w<strong>in</strong>dow of human<br />
VEGF may be different than <strong>in</strong>dicated by precl<strong>in</strong>ical studies with mur<strong>in</strong>e VEGF, highlight<strong>in</strong>g the<br />
need for rigorous safety test<strong>in</strong>g <strong>in</strong> Stage I cl<strong>in</strong>ical trials.<br />
44.9<br />
Target<strong>in</strong>g mTORC2 <strong>in</strong>hibits colon cancer cell proliferation <strong>in</strong> vitro and tumor formation <strong>in</strong> vivo<br />
D. Roul<strong>in</strong>, Y. Cerantola, A. Dormond-Meuwly, N. Demart<strong>in</strong>es, O. Dormond (Lausanne)<br />
Objective: The mammalian target of rapamyc<strong>in</strong> (mTOR), which exists <strong>in</strong> two functionally dist<strong>in</strong>ct complexes,<br />
mTORC1 and mTORC2, plays an important role <strong>in</strong> tumor growth. Whereas the role of mTORC1<br />
has been well characterized <strong>in</strong> this process, little is known about the functions of mTORC2 <strong>in</strong> cancer<br />
progression. This present study aims at explor<strong>in</strong>g the specific role of mTORC2 <strong>in</strong> colon cancer progression.<br />
Methods: A short hairp<strong>in</strong> RNA expression system was used to silence the mTORC2-associated prote<strong>in</strong><br />
rictor.<br />
Results: We observed that downregulation of rictor <strong>in</strong> HT29 and LS174T colon cancer cells significantly<br />
reduced cell proliferation. Knockdown of rictor also resulted <strong>in</strong> a G1 arrest as observed by cell cycle<br />
analysis. We further observed that LS174T cells deficient for rictor failed to form tumors <strong>in</strong> a nude mice<br />
xenograft model.<br />
Conclusion: Taken together, these results show that the <strong>in</strong>hibition of mTORC2 reduces colon cancer<br />
cell proliferation <strong>in</strong> vitro and tumor xenograft formation <strong>in</strong> vivo. They also suggest that specifically target<strong>in</strong>g<br />
mTORC2 may provide a novel treatment strategy for colorectal cancer.<br />
Cardiac Surgery 45<br />
45.1<br />
Aortic-valve spar<strong>in</strong>g or aortic root replacement: experience over 48 consecutive patients<br />
P. Matt, B. W<strong>in</strong>kler, F. Rüter, M. Grapow, O. Reuthebuch, F. Eckste<strong>in</strong> (Basel)<br />
Objective: Controversy exists on how often aortic-valve spar<strong>in</strong>g can be performed <strong>in</strong> case of aortic<br />
root surgery.<br />
Methods: We report our experience over 48 consecutive patients operated for aortic root disease from<br />
July 2008 to December 2009.<br />
Results: 11 (23%) patients underwent aortic-valve spar<strong>in</strong>g (AVS; mean age 59.2 years; 9 males) and<br />
37 (77%) composite-graft replacement (CG; 53.6 years; 33 males; P=0.1, P=0.8). Preoperative logistic<br />
Euroscore was 16.3 (AVS) and 21.4 (CG; P=0.4). There were 11 redo-procedures and 2 homografts<br />
(CG), no such <strong>in</strong> the AVS group. Emergent procedures were performed <strong>in</strong> 3 (AVS) and 6 (CG; P=0.7).<br />
Aortic valve regurgitation was moderate or severe <strong>in</strong> 9 (AVS) and 23 (CG; P=0.4). Aortic valve stenosis<br />
had 10 patients <strong>in</strong> the CG group, none <strong>in</strong> the AVS. Deep hypothermic circulatory arrest (DHCA) was<br />
performed <strong>in</strong> 8 (AVS) and 30 (CG; P=0.8). Hemiarch and arch replacement was done <strong>in</strong> 5 and 3 AVS<br />
patients, respectively, and <strong>in</strong> 23 and 0 of those with CG. DHCA time was 17.6 m<strong>in</strong> (AVS) and 24 m<strong>in</strong><br />
(CG; P=0.0). Ischemic and perfusion time was 134.8 m<strong>in</strong> and 158.8 m<strong>in</strong> (AVS), and 119 m<strong>in</strong> and<br />
168 m<strong>in</strong> (CG; P=0.2, P=0.7). Deepest temperature was 26 degree (AVS) and 23 degree (CG; P=0.3).<br />
Intensive care unit time was 2.7 days (AVS) and 3.4 days (CG; P=0.6). Stroke occurred <strong>in</strong> 2 (AVS) and<br />
3 (CG; P=0.6). Pneumonia or pulmonary embolism showed 1 (AVS) and 3 (CG) patients (P=1). At<br />
discharge, AVS patients showed no (n=10) or mild (n=1) aortic valve <strong>in</strong>sufficiency. 30-day mortality<br />
was 0% <strong>in</strong> AVS patients, and 8% <strong>in</strong> CG patients (3 of 37, one patient died due to <strong>in</strong>test<strong>in</strong>al ischemia, two<br />
patients due to multi-<strong>org</strong>an failure).<br />
Conclusion: AVS was performed <strong>in</strong> 23% of consecutive aortic root procedures with excellent results.<br />
Operative risk of AVS and CG is low, even if comb<strong>in</strong>ed with hemiarch or arch surgery.<br />
45.2<br />
Aortic root replacement with cryopreserved homografts <strong>in</strong> prosthetic valve endocarditis<br />
F. Rüter, B. W<strong>in</strong>kler, M. T. Grapow, P. Matt, O. Reuthebuch, F. Eckste<strong>in</strong> (Basel)<br />
Objective: Prosthetic valve endocarditis rema<strong>in</strong>s a serious disorder after aortic valve replacement<br />
(AVR) despite novel antibiotic regimens. In case of extensive abscess formation, rhythm disorders or<br />
non respond<strong>in</strong>g to drug therapy, surgical <strong>in</strong>tervention rema<strong>in</strong>s as only curative treatment. For these<br />
patients, cryopreserved homografts are <strong>in</strong>creas<strong>in</strong>gly used for aortic root and valve replacement.<br />
Methods: We report five consecutive patients who required reoperation after AVR due to severe endocarditis.<br />
In cooperation with the European Homograft Bank (Brussels, Belgium) the homograft program<br />
has been set up accord<strong>in</strong>g to National Health Comission standards. Infrastructure, tra<strong>in</strong><strong>in</strong>g of<br />
staff and follow-up guidel<strong>in</strong>es were established at our <strong>in</strong>stitute.<br />
Results: All operations were performed <strong>in</strong> full root technique, a partial replacement of the anterior mitral<br />
valve leaflet was additionally necessary <strong>in</strong> one case. All patients were <strong>in</strong>cluded <strong>in</strong> a retrospective<br />
survey with echocardiographic and cl<strong>in</strong>ical checkups before discharge and 6 months postoperatively.<br />
No patient has evidence for persistent <strong>in</strong>fection or required reoperation. All patients recovered to full<br />
extend.<br />
Conclusion: In prosthetic aortic valve endocarditis with annulus destruction or <strong>in</strong>volvement of the an-<br />
terior mitral valve leaflet, homograft aortic root replacement appears to show the best outcome and<br />
comb<strong>in</strong>es avoidance of anticoagulation, best hemodynamic function and resistance to <strong>in</strong>fection.<br />
45.3<br />
Fluid dynamics <strong>in</strong> aortic valve bioprostheses: a novel approach<br />
T. Syburra, A. Landolt, T. Rösgen, D. Obrist, M. Genoni (Zurich)<br />
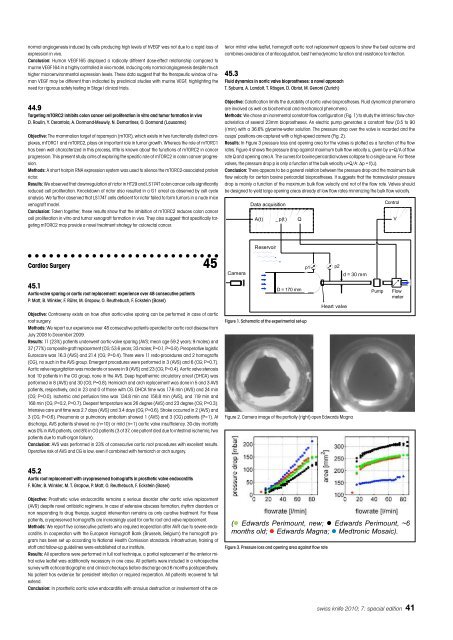
Objective: Calcification limits the durability of aortic valve bioprostheses. Fluid dynamical phenomena<br />
are <strong>in</strong>volved as well as biochemical and mechanical phenomena.<br />
Methods: We chose an <strong>in</strong>cremental constant-flow configuration (Fig. 1) to study the <strong>in</strong>tr<strong>in</strong>sic flow characteristics<br />
of several 23mm bioprostheses. An electric pump generates a constant flow (0.5 to 90<br />
l/m<strong>in</strong>) with a 36.6% glycer<strong>in</strong>e-water solution. The pressure drop over the valve is recorded and the<br />
cusps’ positions are captured with a high-speed camera (Fig. 2).<br />
Results: In Figure 3 pressure loss and open<strong>in</strong>g area for the valves is plotted as a function of the flow<br />
rates. Figure 4 shows the pressure drop aga<strong>in</strong>st maximum bulk flow velocity u, given by u=Q/A of flow<br />
rate Q and open<strong>in</strong>g area A. The curves for bov<strong>in</strong>e pericardial valves collapse to a s<strong>in</strong>gle curve. For these<br />
valves, the pressure drop p is only a function of the bulk velocity u=Q/A: Δp = f(u).<br />
Conclusion: There appears to be a general relation between the pressure drop and the maximum bulk<br />
flow velocity for certa<strong>in</strong> bov<strong>in</strong>e pericardial bioprostheses. It suggests that the transvalvular pressure<br />
drop is ma<strong>in</strong>ly a function of the maximum bulk flow velocity and not of the flow rate. Valves should<br />
be designed to yield large open<strong>in</strong>g areas already at low flow rates m<strong>in</strong>imiz<strong>in</strong>g the bulk flow velocity.<br />
������<br />
���� �����������<br />
���� ����� �<br />
���������<br />
����������<br />
Figure 1. Schematic of the experimental set-up<br />
��<br />
��<br />
����� �����<br />
Figure 2. Camera image of the partially (right) open Edwards Magna<br />
���������<br />
����<br />
�������<br />
swiss <strong>knife</strong> 2010; 7: special edition 41<br />
�<br />
����<br />
�����<br />
�<br />
���������������������������������������������������������<br />
��� ������������������������ �� ����������������������<br />
��������������������������������������������������<br />
��� ������������������������ �� ����������������������<br />
������ ���� � ������� ������ � ��������� �������<br />
Figure 3. Pressure loss and open<strong>in</strong>g area aga<strong>in</strong>st flow rate<br />
�