Anorectal Manometry in 3D NEW! - Swiss-knife.org
Anorectal Manometry in 3D NEW! - Swiss-knife.org
Anorectal Manometry in 3D NEW! - Swiss-knife.org
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
62.7<br />
Posttraumatic symptomatic cystic adventitial degeneration (CAD) of the radial artery: an unusual<br />
localization<br />
C. Rouden 1 , T. Wolff 1 , T. Eugster 1 , L. Gürke 1 , P. Stierli 1,3 , C. Jeanneret 2 , C. Koella 2 ( 1 Basel, 2 Bruderholz,<br />
3 Aarau)<br />
Objective: Cystic adventitial disease (CAD) is a rare cause of non-atherosclerotic stenosis and one of<br />
the ma<strong>in</strong> reasons for claudication <strong>in</strong> young and middle-aged men. Because of the rarity of the disease,<br />
it is often unrecognized and frequently mistaken for atherosclerotic disease. The localization <strong>in</strong> the<br />
wrist is very rare.<br />
Methods: We report a case of <strong>in</strong> a 45-year old man, who fell on his left extended hand due to a motorcycle<br />
accident. In the follow<strong>in</strong>g weeks a pa<strong>in</strong>ful grow<strong>in</strong>g mass developed on the radial side of his left<br />
wrist. Cl<strong>in</strong>ical exam<strong>in</strong>ation revealed a one centimeter elastic mass at the palmar aspect of the wrist,<br />
very tender at palpation. No <strong>in</strong>fection signs and no impaired distal perfusion could be detected. The<br />
conventional x-ray excluded a fracture. The duplex exam<strong>in</strong>ation showed a cyst (1,8x 0,6x 1 cm) shift<strong>in</strong>g<br />
and slightly compress<strong>in</strong>g the radial artery. The oscillogram was normal and symmetrical on both<br />
arms. The CT-angiogram confirmed the suspicion of CAD (scimitar sign).<br />
Results: At the operation an outly<strong>in</strong>g small elastic mass conf<strong>in</strong>ed to the wall of the artery itself was prepared.<br />
After exarterectomy, leav<strong>in</strong>g just the media <strong>in</strong> situ, we found a f<strong>in</strong>e connection between the CAD<br />
to the radio-carpal articulation. The cyst conta<strong>in</strong>ed gelat<strong>in</strong>ous substance. The patient had an uneventful<br />
postoperative recovery and was discharged on the first postoperative day. The cl<strong>in</strong>ical and duplex<br />
controls at three months were normal and 3 years later the patient was still free of recurrent disease.<br />
Conclusion: CAD is generally located to the popliteal artery, although it may be found <strong>in</strong> other arteries<br />
and even <strong>in</strong> ve<strong>in</strong>s. Histologically it consists of a collection of gelat<strong>in</strong>ous material with<strong>in</strong> a cyst adjacent<br />
to or surround<strong>in</strong>g a vessel. The treatment of choice is surgical removal of the cyst or reconstruction<br />
with autologous ve<strong>in</strong> or synthetic graft <strong>in</strong>terposition. Percutaneous ultrasound-guided cystic aspiration<br />
is an alternative method for treat<strong>in</strong>g the disease but may result <strong>in</strong> local recurrence. The etiology is still<br />
unclear: most authors believe that CAD may orig<strong>in</strong>ate from an ectopic synovial ganglion close to the<br />
adjacent jo<strong>in</strong>t capsule. In our case we found a communication between the cyst and the radio-carpal<br />
jo<strong>in</strong>t, support<strong>in</strong>g this theory.<br />
62.8<br />
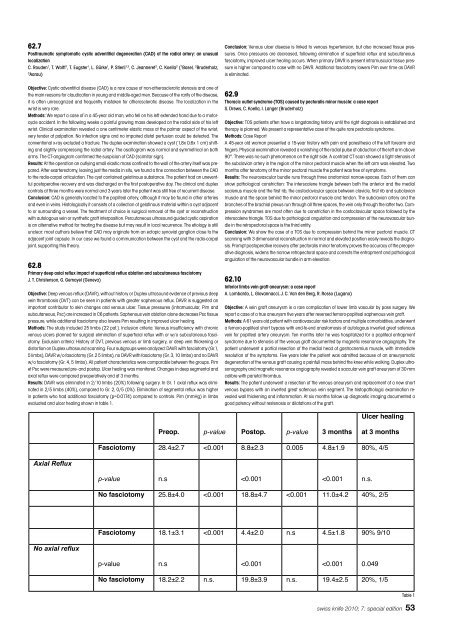
Primary deep axial reflux impact of superficial reflux ablation and subcutaneous fasciotomy<br />
J. T. Christenson, G. Gemayel (Geneva)<br />
Objective: Deep venous reflux (DAVR), without history or Duplex ultrasound evidence of previous deep<br />
ve<strong>in</strong> thrombosis (DVT) can be seen <strong>in</strong> patients with greater saphenous reflux. DAVR is suggested an<br />
important contributor to sk<strong>in</strong> changes and venous ulcer. Tissue pressures (<strong>in</strong>tramuscular, Pim and<br />
subcutaneous, Psc) are <strong>in</strong>creased <strong>in</strong> C6 patients. Saphenous ve<strong>in</strong> ablation alone decreases Psc tissue<br />
pressure, while additional fasciotomy also lowers Pim result<strong>in</strong>g <strong>in</strong> improved ulcer heal<strong>in</strong>g.<br />
Methods: The study <strong>in</strong>cluded 25 limbs (22 pat.). Inclusion criteria: Venous <strong>in</strong>sufficiency with chronic<br />
venous ulcers planned for surgical elim<strong>in</strong>ation of superficial reflux with or w/o subcutaneous fasciotomy.<br />
Exclusion criteria: History of DVT, previous venous or limb surgery, or deep ve<strong>in</strong> thicken<strong>in</strong>g or<br />
distortion on Duplex ultrasound scann<strong>in</strong>g. Four subgroups were analyzed: DAVR with fasciotomy (Gr.1,<br />
5 limbs), DAVR w/o fasciotomy (Gr. 2 5 limbs), no DAVR with fasciotomy (Gr. 3, 10 limbs) and no DAVR<br />
w/o fasciotomy (Gr. 4, 5 limbs). All patient characteristics were comparable between the groups. Pim<br />
et Psc were measured pre- and postop. Ulcer heal<strong>in</strong>g was monitored. Changes <strong>in</strong> deep segmental and<br />
axial reflux were compared preoperatively and at 3 months.<br />
Results: DAVR was elim<strong>in</strong>ated <strong>in</strong> 2/10 limbs (20%) follow<strong>in</strong>g surgery. In Gr. 1 axial reflux was elim<strong>in</strong>ated<br />
<strong>in</strong> 2/5 limbs (40%), compared to Gr. 2, 0/5 (0%). Elim<strong>in</strong>ation of segmental reflux was higher<br />
<strong>in</strong> patients who had additional fasciotomy (p=0.0174) compared to controls. Pim (mmHg) <strong>in</strong> limbs<br />
evaluated and ulcer heal<strong>in</strong>g shown <strong>in</strong> table 1.<br />
� � �<br />
�������������<br />
����������������<br />
Conclusion: Venous ulcer disease is l<strong>in</strong>ked to venous hypertension, but also <strong>in</strong>creased tissue pressures.<br />
Once pressures are decreased, follow<strong>in</strong>g elim<strong>in</strong>ation of superficial reflux and subcutaneous<br />
fasciotomy, improved ulcer heal<strong>in</strong>g occurs. When primary DAVR is present <strong>in</strong>tramuscular tissue pressure<br />
is higher compared to case with no DAVR. Additional fasciotomy lowers Pim over time as DAVR<br />
is elim<strong>in</strong>ated.<br />
62.9<br />
Thoracic outlet syndrome (TOS) caused by pectoralis m<strong>in</strong>or muscle: a case report<br />
S. Drews, C. Koella, I. Langer (Bruderholz)<br />
Objective: TOS patients often have a longstand<strong>in</strong>g history until the right diagnosis is established and<br />
therapy is planned. We present a representative case of the quite rare pectoralis syndrome.<br />
Methods: Case Report<br />
A 45-year old woman presented a 15-year history with pa<strong>in</strong> and paresthesia of the left forearm and<br />
f<strong>in</strong>gers. Physical exam<strong>in</strong>ation revealed a vanish<strong>in</strong>g of the radial pulse at abduction of the left arm above<br />
90°. There was no such phenomenon on the right side. A contrast CT scan showed a tight stenosis of<br />
the subclavian artery <strong>in</strong> the region of the m<strong>in</strong>or pectoral muscle when the left arm was elevated. Two<br />
months after tenotomy of the m<strong>in</strong>or pectoral muscle the patient was free of symptoms.<br />
Results: The neurovascular bundle runs through three anatomical narrow-spaces. Each of them can<br />
show pathological constriction: The <strong>in</strong>terscalene triangle between both the anterior and the medial<br />
scalenus muscle and the first rib, the costoclavicular space between clavicle, first rib and subclavian<br />
muscle and the space beh<strong>in</strong>d the m<strong>in</strong>or pectoral muscle and tendon. The subclavian artery and the<br />
branches of the brachial plexus run through all three spaces, the ve<strong>in</strong> only through the latter two. Compression<br />
syndromes are most often due to constriction <strong>in</strong> the costoclavicular space followed by the<br />
<strong>in</strong>terscalene triangle. TOS due to pathological angulation and compression of the neurovascular bundle<br />
<strong>in</strong> the retropectoral space is the third entity.<br />
Conclusion: We show the case of a TOS due to compression beh<strong>in</strong>d the m<strong>in</strong>or pectoral muscle. CT<br />
scann<strong>in</strong>g with 3 dimensional reconstruction <strong>in</strong> normal and elevated position easily reveals the diagnosis.<br />
Prompt postoperative recovery after pectoralis m<strong>in</strong>or tenotomy proves the accuracy of the preoperative<br />
diagnosis, widens the narrow retropectoral space and corrects the entrapment and pathological<br />
angulation of the neurovascular bundle <strong>in</strong> arm elevation.<br />
62.10<br />
Inferior limbs ve<strong>in</strong> graft aneurysm: a case report<br />
A. Lombardo, L. Giovannacci, J. C. Van den Berg, R. Rosso (Lugano)<br />
Objective: A ve<strong>in</strong> graft aneurysm is a rare complication of lower limb vascular by pass surgery. We<br />
report a case of a true aneurysm five years after reversed femoro-popliteal saphenous ve<strong>in</strong> graft.<br />
Methods: A 61 years old patient with cardiovascular risk factors and multiple comorbidities, underwent<br />
a femoro-popliteal short bypass with end-to-end anastomosis of autologous <strong>in</strong>verted great safenous<br />
ve<strong>in</strong> for popliteal artery aneurysm. Ten months later he was hospitalized for a popliteal entrapment<br />
syndrome due to stenosis of the venous graft documented by magnetic resonance angiography. The<br />
patient underwent a partial resection of the medial head of gastrocnemius muscle, with immediate<br />
resolution of the symptoms. Five years later the patient was admitted because of an aneurysmatic<br />
degeneration of the venous graft caus<strong>in</strong>g a pa<strong>in</strong>full mass beh<strong>in</strong>d the knee while walk<strong>in</strong>g. Duplex ultrasonography<br />
and magnetic resonance angiography revealed a saccular ve<strong>in</strong> graft aneurysm of 30 mm<br />
calibre with parietal thrombus.<br />
Results: The patient underwent a resection of the venous aneurysm and replacement of a new short<br />
venous bypass with an <strong>in</strong>verted great safenous ve<strong>in</strong> segment. The histopathologic exam<strong>in</strong>ation revealed<br />
wall thicken<strong>in</strong>g and <strong>in</strong>flammation. At six months follow up diagnostic imag<strong>in</strong>g documented a<br />
good patency without restenosis or dilatations of the graft.<br />
������� �������� �������� �������� ���������<br />
��������������<br />
������������<br />
����������� ��������� ������� �������� ������ �������� ���������<br />
�������� ����<br />
� �<br />
�������<br />
� �<br />
������� �����<br />
�������������� ��������� ������� ��������� ������� ��������� ���������<br />
� � � � � �<br />
����������� ��������� ������� �������� ���� �������� ���������<br />
�������� ����<br />
� �<br />
�������<br />
� �<br />
������� ������<br />
�������������� ��������� ����� ��������� ����� ��������� ���������<br />
Table 1<br />
swiss <strong>knife</strong> 2010; 7: special edition 53