Aanesthetic Agents for Day Surgery - NIHR Health Technology ...
Aanesthetic Agents for Day Surgery - NIHR Health Technology ...
Aanesthetic Agents for Day Surgery - NIHR Health Technology ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
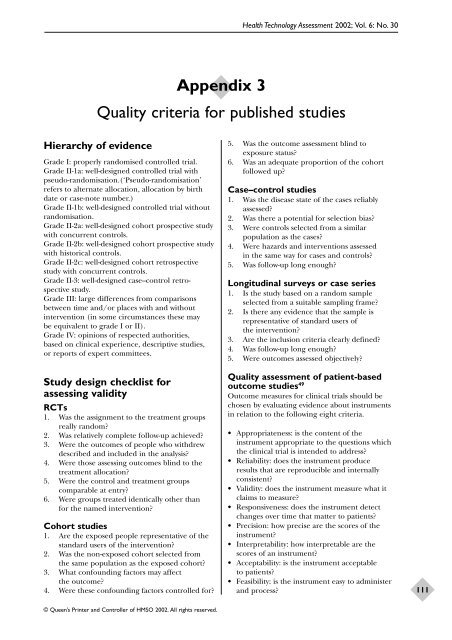
Hierarchy of evidence<br />
Grade I: properly randomised controlled trial.<br />
Grade II-1a: well-designed controlled trial with<br />
pseudo-randomisation.(‘Pseudo-randomisation’<br />
refers to alternate allocation, allocation by birth<br />
date or case-note number.)<br />
Grade II-1b: well-designed controlled trial without<br />
randomisation.<br />
Grade II-2a: well-designed cohort prospective study<br />
with concurrent controls.<br />
Grade II-2b: well-designed cohort prospective study<br />
with historical controls.<br />
Grade II-2c: well-designed cohort retrospective<br />
study with concurrent controls.<br />
Grade II-3: well-designed case–control retrospective<br />
study.<br />
Grade III: large differences from comparisons<br />
between time and/or places with and without<br />
intervention (in some circumstances these may<br />
be equivalent to grade I or II).<br />
Grade IV: opinions of respected authorities,<br />
based on clinical experience, descriptive studies,<br />
or reports of expert committees.<br />
Study design checklist <strong>for</strong><br />
assessing validity<br />
RCTs<br />
1. Was the assignment to the treatment groups<br />
really random?<br />
2. Was relatively complete follow-up achieved?<br />
3. Were the outcomes of people who withdrew<br />
described and included in the analysis?<br />
4. Were those assessing outcomes blind to the<br />
treatment allocation?<br />
5. Were the control and treatment groups<br />
comparable at entry?<br />
6. Were groups treated identically other than<br />
<strong>for</strong> the named intervention?<br />
Cohort studies<br />
1. Are the exposed people representative of the<br />
standard users of the intervention?<br />
2. Was the non-exposed cohort selected from<br />
the same population as the exposed cohort?<br />
3. What confounding factors may affect<br />
the outcome?<br />
4. Were these confounding factors controlled <strong>for</strong>?<br />
© Queen’s Printer and Controller of HMSO 2002. All rights reserved.<br />
Appendix 3<br />
<strong>Health</strong> <strong>Technology</strong> Assessment 2002; Vol. 6: No. 30<br />
Quality criteria <strong>for</strong> published studies<br />
5. Was the outcome assessment blind to<br />
exposure status?<br />
6. Was an adequate proportion of the cohort<br />
followed up?<br />
Case–control studies<br />
1. Was the disease state of the cases reliably<br />
assessed?<br />
2. Was there a potential <strong>for</strong> selection bias?<br />
3. Were controls selected from a similar<br />
population as the cases?<br />
4. Were hazards and interventions assessed<br />
in the same way <strong>for</strong> cases and controls?<br />
5. Was follow-up long enough?<br />
Longitudinal surveys or case series<br />
1. Is the study based on a random sample<br />
selected from a suitable sampling frame?<br />
2. Is there any evidence that the sample is<br />
representative of standard users of<br />
the intervention?<br />
3. Are the inclusion criteria clearly defined?<br />
4. Was follow-up long enough?<br />
5. Were outcomes assessed objectively?<br />
Quality assessment of patient-based<br />
outcome studies 49<br />
Outcome measures <strong>for</strong> clinical trials should be<br />
chosen by evaluating evidence about instruments<br />
in relation to the following eight criteria.<br />
• Appropriateness: is the content of the<br />
instrument appropriate to the questions which<br />
the clinical trial is intended to address?<br />
• Reliability: does the instrument produce<br />
results that are reproducible and internally<br />
consistent?<br />
• Validity: does the instrument measure what it<br />
claims to measure?<br />
• Responsiveness: does the instrument detect<br />
changes over time that matter to patients?<br />
• Precision: how precise are the scores of the<br />
instrument?<br />
• Interpretability: how interpretable are the<br />
scores of an instrument?<br />
• Acceptability: is the instrument acceptable<br />
to patients?<br />
• Feasibility: is the instrument easy to administer<br />
and process?<br />
111