Aanesthetic Agents for Day Surgery - NIHR Health Technology ...
Aanesthetic Agents for Day Surgery - NIHR Health Technology ...
Aanesthetic Agents for Day Surgery - NIHR Health Technology ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
• Late recovery<br />
– time to walk unaided<br />
– ability to walk in a straight line<br />
– time to discharge home.<br />
• Psychomotor recovery<br />
– digital symbol substitution test<br />
–P-deletion test (and its variants)<br />
– dot tracking on a computer screen<br />
–Trieger dot test<br />
–critical flicker fusion threshold<br />
– mood adjective checklist<br />
– perceptual accuracy tests<br />
– picture cards recall<br />
– word association or recall<br />
– perceptual memory<br />
– pegboard test<br />
– simple reaction time<br />
– choice reaction time<br />
– body sway coordination tests<br />
– finger tapping<br />
–Maddox Wing<br />
– Aldrete score (postanaesthesia recovery score<br />
looking at activity, respiration, circulation,<br />
consciousness and colour).<br />
• Unwanted side-effects<br />
–PONV<br />
– pain (visual analogue scale (VAS) scores)<br />
– anxiety (VAS scores).<br />
Adult clinical review<br />
This section examines research on the impact of<br />
anaesthesia techniques in day surgery on adult<br />
clinical outcomes.<br />
Summary of clinical evidence<br />
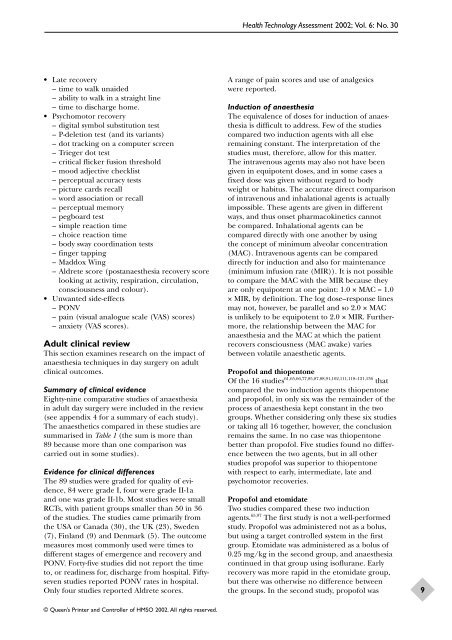
Eighty-nine comparative studies of anaesthesia<br />
in adult day surgery were included in the review<br />
(see appendix 4 <strong>for</strong> a summary of each study).<br />
The anaesthetics compared in these studies are<br />
summarised in Table 1 (the sum is more than<br />
89 because more than one comparison was<br />
carried out in some studies).<br />
Evidence <strong>for</strong> clinical differences<br />
The 89 studies were graded <strong>for</strong> quality of evidence,<br />
84 were grade I, four were grade II-1a<br />
and one was grade II-1b. Most studies were small<br />
RCTs, with patient groups smaller than 50 in 36<br />
of the studies. The studies came primarily from<br />
the USA or Canada (30), the UK (23), Sweden<br />
(7), Finland (9) and Denmark (5). The outcome<br />
measures most commonly used were times to<br />
different stages of emergence and recovery and<br />
PONV. Forty-five studies did not report the time<br />
to, or readiness <strong>for</strong>, discharge from hospital. Fiftyseven<br />
studies reported PONV rates in hospital.<br />
Only four studies reported Aldrete scores.<br />
© Queen’s Printer and Controller of HMSO 2002. All rights reserved.<br />
<strong>Health</strong> <strong>Technology</strong> Assessment 2002; Vol. 6: No. 30<br />
A range of pain scores and use of analgesics<br />
were reported.<br />
Induction of anaesthesia<br />
The equivalence of doses <strong>for</strong> induction of anaesthesia<br />
is difficult to address. Few of the studies<br />
compared two induction agents with all else<br />
remaining constant. The interpretation of the<br />
studies must, there<strong>for</strong>e, allow <strong>for</strong> this matter.<br />
The intravenous agents may also not have been<br />
given in equipotent doses, and in some cases a<br />
fixed dose was given without regard to body<br />
weight or habitus. The accurate direct comparison<br />
of intravenous and inhalational agents is actually<br />
impossible. These agents are given in different<br />
ways, and thus onset pharmacokinetics cannot<br />
be compared. Inhalational agents can be<br />
compared directly with one another by using<br />
the concept of minimum alveolar concentration<br />
(MAC). Intravenous agents can be compared<br />
directly <strong>for</strong> induction and also <strong>for</strong> maintenance<br />
(minimum infusion rate (MIR)). It is not possible<br />
to compare the MAC with the MIR because they<br />
are only equipotent at one point: 1.0 × MAC = 1.0<br />
× MIR, by definition. The log dose–response lines<br />
may not, however, be parallel and so 2.0 × MAC<br />
is unlikely to be equipotent to 2.0 × MIR. Furthermore,<br />
the relationship between the MAC <strong>for</strong><br />
anaesthesia and the MAC at which the patient<br />
recovers consciousness (MAC awake) varies<br />
between volatile anaesthetic agents.<br />
Propofol and thiopentone<br />
Of the 16 studies 61,65,66,77,85,87,88,91,102,111,118–121,136 that<br />
compared the two induction agents thiopentone<br />
and propofol, in only six was the remainder of the<br />
process of anaesthesia kept constant in the two<br />
groups. Whether considering only these six studies<br />
or taking all 16 together, however, the conclusion<br />
remains the same. In no case was thiopentone<br />
better than propofol. Five studies found no difference<br />
between the two agents, but in all other<br />
studies propofol was superior to thiopentone<br />
with respect to early, intermediate, late and<br />
psychomotor recoveries.<br />
Propofol and etomidate<br />
Two studies compared these two induction<br />
agents. 65,97 The first study is not a well-per<strong>for</strong>med<br />
study. Propofol was administered not as a bolus,<br />
but using a target controlled system in the first<br />
group. Etomidate was administered as a bolus of<br />
0.25 mg/kg in the second group, and anaesthesia<br />
continued in that group using isoflurane. Early<br />
recovery was more rapid in the etomidate group,<br />
but there was otherwise no difference between<br />
the groups. In the second study, propofol was<br />
9