A systematic review and economic model of the effectiveness and ...
A systematic review and economic model of the effectiveness and ...
A systematic review and economic model of the effectiveness and ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
92<br />
Review <strong>of</strong> <strong>economic</strong> evaluations <strong>of</strong> ADHD drug interventions in children <strong>and</strong> adolescents<br />
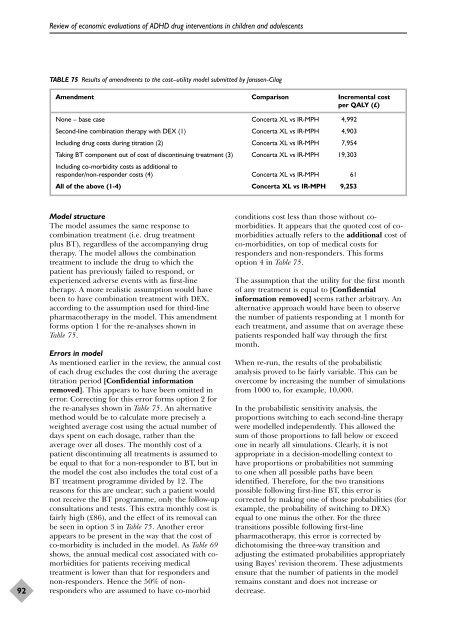
TABLE 75 Results <strong>of</strong> amendments to <strong>the</strong> cost–utility <strong>model</strong> submitted by Janssen-Cilag<br />
Amendment Comparison Incremental cost<br />
per QALY (£)<br />
None – base case Concerta XL vs IR-MPH 4,992<br />
Second-line combination <strong>the</strong>rapy with DEX (1) Concerta XL vs IR-MPH 4,903<br />
Including drug costs during titration (2) Concerta XL vs IR-MPH 7,954<br />
Taking BT component out <strong>of</strong> cost <strong>of</strong> discontinuing treatment (3)<br />
Including co-morbidity costs as additional to<br />
Concerta XL vs IR-MPH 19,303<br />
responder/non-responder costs (4) Concerta XL vs IR-MPH 61<br />
All <strong>of</strong> <strong>the</strong> above (1-4) Concerta XL vs IR-MPH 9,253<br />
Model structure<br />
The <strong>model</strong> assumes <strong>the</strong> same response to<br />
combination treatment (i.e. drug treatment<br />
plus BT), regardless <strong>of</strong> <strong>the</strong> accompanying drug<br />
<strong>the</strong>rapy. The <strong>model</strong> allows <strong>the</strong> combination<br />
treatment to include <strong>the</strong> drug to which <strong>the</strong><br />
patient has previously failed to respond, or<br />
experienced adverse events with as first-line<br />
<strong>the</strong>rapy. A more realistic assumption would have<br />
been to have combination treatment with DEX,<br />
according to <strong>the</strong> assumption used for third-line<br />
pharmaco<strong>the</strong>rapy in <strong>the</strong> <strong>model</strong>. This amendment<br />
forms option 1 for <strong>the</strong> re-analyses shown in<br />
Table 75.<br />
Errors in <strong>model</strong><br />
As mentioned earlier in <strong>the</strong> <strong>review</strong>, <strong>the</strong> annual cost<br />
<strong>of</strong> each drug excludes <strong>the</strong> cost during <strong>the</strong> average<br />
titration period [Confidential information<br />
removed]. This appears to have been omitted in<br />
error. Correcting for this error forms option 2 for<br />
<strong>the</strong> re-analyses shown in Table 75. An alternative<br />
method would be to calculate more precisely a<br />
weighted average cost using <strong>the</strong> actual number <strong>of</strong><br />
days spent on each dosage, ra<strong>the</strong>r than <strong>the</strong><br />
average over all doses. The monthly cost <strong>of</strong> a<br />
patient discontinuing all treatments is assumed to<br />
be equal to that for a non-responder to BT, but in<br />
<strong>the</strong> <strong>model</strong> <strong>the</strong> cost also includes <strong>the</strong> total cost <strong>of</strong> a<br />
BT treatment programme divided by 12. The<br />
reasons for this are unclear; such a patient would<br />
not receive <strong>the</strong> BT programme, only <strong>the</strong> follow-up<br />
consultations <strong>and</strong> tests. This extra monthly cost is<br />
fairly high (£86), <strong>and</strong> <strong>the</strong> effect <strong>of</strong> its removal can<br />
be seen in option 3 in Table 75. Ano<strong>the</strong>r error<br />
appears to be present in <strong>the</strong> way that <strong>the</strong> cost <strong>of</strong><br />
co-morbidity is included in <strong>the</strong> <strong>model</strong>. As Table 69<br />
shows, <strong>the</strong> annual medical cost associated with comorbidities<br />
for patients receiving medical<br />
treatment is lower than that for responders <strong>and</strong><br />
non-responders. Hence <strong>the</strong> 50% <strong>of</strong> nonresponders<br />
who are assumed to have co-morbid<br />
conditions cost less than those without comorbidities.<br />
It appears that <strong>the</strong> quoted cost <strong>of</strong> comorbidities<br />
actually refers to <strong>the</strong> additional cost <strong>of</strong><br />
co-morbidities, on top <strong>of</strong> medical costs for<br />
responders <strong>and</strong> non-responders. This forms<br />
option 4 in Table 75.<br />
The assumption that <strong>the</strong> utility for <strong>the</strong> first month<br />
<strong>of</strong> any treatment is equal to [Confidential<br />
information removed] seems ra<strong>the</strong>r arbitrary. An<br />
alternative approach would have been to observe<br />
<strong>the</strong> number <strong>of</strong> patients responding at 1 month for<br />
each treatment, <strong>and</strong> assume that on average <strong>the</strong>se<br />
patients responded half way through <strong>the</strong> first<br />
month.<br />
When re-run, <strong>the</strong> results <strong>of</strong> <strong>the</strong> probabilistic<br />
analysis proved to be fairly variable. This can be<br />
overcome by increasing <strong>the</strong> number <strong>of</strong> simulations<br />
from 1000 to, for example, 10,000.<br />
In <strong>the</strong> probabilistic sensitivity analysis, <strong>the</strong><br />
proportions switching to each second-line <strong>the</strong>rapy<br />
were <strong>model</strong>led independently. This allowed <strong>the</strong><br />
sum <strong>of</strong> those proportions to fall below or exceed<br />
one in nearly all simulations. Clearly, it is not<br />
appropriate in a decision-<strong>model</strong>ling context to<br />
have proportions or probabilities not summing<br />
to one when all possible paths have been<br />
identified. Therefore, for <strong>the</strong> two transitions<br />
possible following first-line BT, this error is<br />
corrected by making one <strong>of</strong> those probabilities (for<br />
example, <strong>the</strong> probability <strong>of</strong> switching to DEX)<br />
equal to one minus <strong>the</strong> o<strong>the</strong>r. For <strong>the</strong> three<br />
transitions possible following first-line<br />
pharmaco<strong>the</strong>rapy, this error is corrected by<br />
dichotomising <strong>the</strong> three-way transition <strong>and</strong><br />
adjusting <strong>the</strong> estimated probabilities appropriately<br />
using Bayes’ revision <strong>the</strong>orem. These adjustments<br />
ensure that <strong>the</strong> number <strong>of</strong> patients in <strong>the</strong> <strong>model</strong><br />
remains constant <strong>and</strong> does not increase or<br />
decrease.