Here - American Geriatrics Society
Here - American Geriatrics Society
Here - American Geriatrics Society
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
P APER<br />
A BSTRACTS<br />
Paper Session<br />
Clinical Decision-Making<br />
Thursday, May 3<br />
7:30 am – 9:00 am<br />
P1<br />
Lagtime to Benefit for Colorectal Cancer Screening: A Survival<br />
Meta-Analysis.<br />
S. J. Lee, 1 W. J. Boscardin, 1,2 I. Stijacic-Cenzer, 1,2 J. Conell-Price, 1<br />
S. O’Brien, 1 L. C. Walter. 1,2 1. Division of <strong>Geriatrics</strong>, SFVAMC, UCSF,<br />
San Francisco, CA; 2. Department of Epidemiology and Biostatistics,<br />
University of California, San Francisco, San Francisco, CA.<br />
Supported By: Dr. Sei Lee was supported by Hartford <strong>Geriatrics</strong><br />
Health Outcomes Research Scholars Award, the Hellman Family<br />
Award for Early Career Faculty at UCSF and the KL2RR024130<br />
from the National Center for Research Resources, a component of<br />
the NIH.<br />
Dr. Louise Walter was supported by R01CA134425 from the<br />
National Cancer Institute, which was administered by the Northern<br />
California Institute for Research and Education.<br />
This work was supported with resources of the Veterans Affairs<br />
Medical Center, San Francisco, California.<br />
Background: Guidelines recommend targeting colorectal cancer<br />
(CRC) screening to healthy patients whose life expectancy exceeds<br />
the cancer screening’s lagtime to benefit (i.e. time between screening<br />
and when the benefits of screening are seen). However, the lagtime of<br />
CRC screening is uncertain. Our goal was to determine a pooled,<br />
quantitative estimate of the lagtime to benefit for CRC screening<br />
from randomized controlled trial (RCT) data.<br />
Methods: We conducted a survival meta-analysis of CRC<br />
screening RCTs focusing on older patients (age greater than 50) identified<br />
by Cochrane and USPSTF reviews as high quality. Four population-based<br />
RCTs of fecal occult blood testing from Denmark, England,<br />
Sweden, and the United States (n=327,043) were included in<br />
our meta-analysis.<br />
Results: 4.9 years (95%CI: 2.1 to 9.5) passed before one CRC<br />
death was prevented for 5000 persons screened (absolute risk reduction<br />
or ARR=0.0002). It took 10.4 years (95%CI: 6.1 to 16.6) before<br />
one CRC death was prevented for 1000 persons screened<br />
(ARR=0.001) and 14.6 years (95%CI: 9.7 to 21.2) for 2 CRC deaths<br />
to be prevented for 1000 persons screened (ARR=0.002).<br />
Conclusions:The lagtime to prevent one CRC death per 1000 persons<br />
screened is 10.4 years suggesting that CRC screening should be<br />
targeted toward patients with a life expectancy greater than ten years.<br />
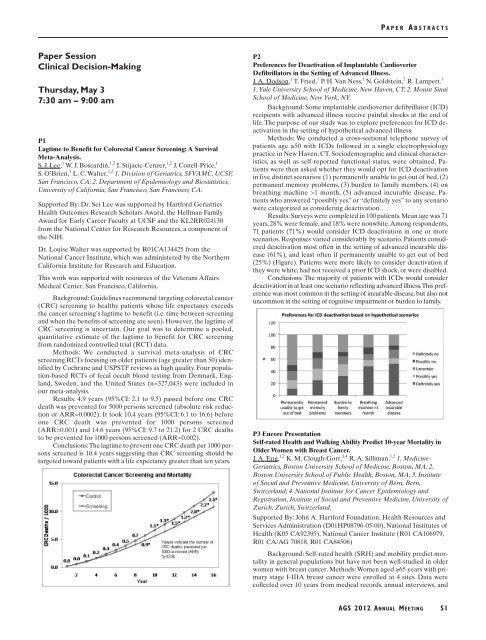
P2<br />
Preferences for Deactivation of Implantable Cardioverter<br />
Defibrillators in the Setting of Advanced Illness.<br />
J. A. Dodson, 1 T. Fried, 1 P. H. Van Ness, 1 N. Goldstein, 2 R. Lampert. 1<br />
1. Yale University School of Medicine, New Haven, CT; 2. Mount Sinai<br />
School of Medicine, New York, NY.<br />
Background: Some implantable cardioverter defibrillator (ICD)<br />
recipients with advanced illness receive painful shocks at the end of<br />
life. The purpose of our study was to explore preferences for ICD deactivation<br />
in the setting of hypothetical advanced illness.<br />
Methods: We conducted a cross-sectional telephone survey of<br />
patients age ≥50 with ICDs followed in a single electrophysiology<br />
practice in New Haven, CT. Sociodemographic and clinical characteristics,<br />
as well as self-reported functional status, were obtained. Patients<br />
were then asked whether they would opt for ICD deactivation<br />
in five distinct scenarios: (1) permanently unable to get out of bed, (2)<br />
permanent memory problems, (3) burden to family members, (4) on<br />
breathing machine >1 month, (5) advanced incurable disease. Patients<br />
who answered “possibly yes” or “definitely yes” to any scenario<br />
were categorized as considering deactivation.<br />
Results: Surveys were completed in 100 patients. Mean age was 71<br />
years, 28% were female, and 18% were nonwhite.Among respondents,<br />
71 patients (71%) would consider ICD deactivation in one or more<br />
scenarios. Responses varied considerably by scenario. Patients considered<br />
deactivation most often in the setting of advanced incurable disease<br />
(61%), and least often if permanently unable to get out of bed<br />
(25%) (Figure). Patients were more likely to consider deactivation if<br />
they were white, had not received a prior ICD shock, or were disabled.<br />
Conclusions: The majority of patients with ICDs would consider<br />
deactivation in at least one scenario reflecting advanced illness.This preference<br />
was most common in the setting of incurable disease, but also not<br />
uncommon in the setting of cognitive impairment or burden to family.<br />
P3 Encore Presentation<br />
Self-rated Health and Walking Ability Predict 10-year Mortality in<br />
Older Women with Breast Cancer.<br />
J. A. Eng, 1,2 K. M. Clough-Gorr, 3,4 R. A. Silliman. 1,2 1. Medicine-<br />
<strong>Geriatrics</strong>, Boston University School of Medicine, Boston, MA; 2.<br />
Boston University School of Public Health, Boston, MA; 3. Institute<br />
of Social and Preventive Medicine, University of Bern, Bern,<br />
Switzerland; 4. National Institute for Cancer Epidemiology and<br />
Registration, Institute of Social and Preventive Medicine, University of<br />
Zurich, Zurich, Switzerland.<br />
Supported By: John A. Hartford Foundation, Health Resources and<br />
Services Administration (D01HP08796-05-00), National Institutes of<br />
Health (K05 CA92395), National Cancer Institute (R01 CA106979,<br />
R01 CA/AG 70818, R01 CA84506)<br />
Background: Self-rated health (SRH) and mobility predict mortality<br />
in general populations but have not been well-studied in older<br />
women with breast cancer. Methods: Women aged ≥65 years with primary<br />
stage I-IIIA breast cancer were enrolled at 4 sites. Data were<br />
collected over 10 years from medical records, annual interviews, and<br />
AGS 2012 ANNUAL MEETING<br />
S1