Supplementum 3+4/2007 - SpoleÄnost pro pojivové tkánÄ›
Supplementum 3+4/2007 - SpoleÄnost pro pojivové tkánÄ›
Supplementum 3+4/2007 - SpoleÄnost pro pojivové tkánÄ›
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
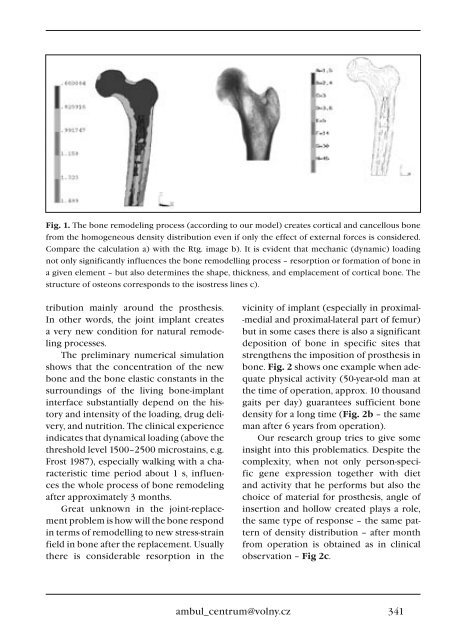
Fig. 1. The bone remodeling <strong>pro</strong>cess (according to our model) creates cortical and cancellous bone<br />
from the homogeneous density distribution even if only the effect of external forces is considered.<br />
Compare the calculation a) with the Rtg. image b). It is evident that mechanic (dynamic) loading<br />
not only significantly influences the bone remodelling <strong>pro</strong>cess – resorption or formation of bone in<br />
a given element – but also determines the shape, thickness, and emplacement of cortical bone. The<br />
structure of osteons corresponds to the isostress lines c).<br />
tribution mainly around the <strong>pro</strong>sthesis.<br />
In other words, the joint implant creates<br />
a very new condition for natural remodeling<br />
<strong>pro</strong>cesses.<br />
The preliminary numerical simulation<br />
shows that the concentration of the new<br />
bone and the bone elastic constants in the<br />
surroundings of the living bone-implant<br />
interface substantially depend on the history<br />
and intensity of the loading, drug delivery,<br />
and nutrition. The clinical experience<br />
indicates that dynamical loading (above the<br />
threshold level 1500–2500 microstains, e.g.<br />
Frost 1987), especially walking with a characteristic<br />
time period about 1 s, influences<br />
the whole <strong>pro</strong>cess of bone remodeling<br />
after ap<strong>pro</strong>ximately 3 months.<br />
Great unknown in the joint-replacement<br />
<strong>pro</strong>blem is how will the bone respond<br />
in terms of remodelling to new stress-strain<br />
field in bone after the replacement. Usually<br />
there is considerable resorption in the<br />
vicinity of implant (especially in <strong>pro</strong>ximal-<br />
-medial and <strong>pro</strong>ximal-lateral part of femur)<br />
but in some cases there is also a significant<br />
deposition of bone in specific sites that<br />
strengthens the imposition of <strong>pro</strong>sthesis in<br />
bone. Fig. 2 shows one example when adequate<br />
physical activity (50-year-old man at<br />
the time of operation, ap<strong>pro</strong>x. 10 thousand<br />
gaits per day) guarantees sufficient bone<br />
density for a long time (Fig. 2b – the same<br />
man after 6 years from operation).<br />
Our research group tries to give some<br />
insight into this <strong>pro</strong>blematics. Despite the<br />
complexity, when not only person-specific<br />
gene expression together with diet<br />
and activity that he performs but also the<br />
choice of material for <strong>pro</strong>sthesis, angle of<br />
insertion and hollow created plays a role,<br />
the same type of response – the same pattern<br />
of density distribution – after month<br />
from operation is obtained as in clinical<br />
observation – Fig 2c.<br />
ambul_centrum@volny.cz<br />
341