The eligibility and enrollment rules for the U
The eligibility and enrollment rules for the U
The eligibility and enrollment rules for the U
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Retiree Health Care SPD Effective January 1, 2012<br />
<strong>the</strong> opportunity to select <strong>the</strong> provider. Examples of this situation include diagnostic lab,<br />
independent diagnostic X-ray <strong>and</strong> independent anes<strong>the</strong>sia providers.<br />
To locate in-network/participating providers, you may ask your provider if he or she participates<br />
with BCBS, call <strong>the</strong> BCBS customer service department, or access <strong>the</strong>ir Web site*. (See <strong>the</strong><br />
“Important Resources” section of this SPD.) In addition, you may call 1-800-810-BLUE (1-800-<br />
810-2583).<br />
It is your responsibility to confirm that <strong>the</strong> provider you use is an in-network/participating<br />
provider.<br />
* Every ef<strong>for</strong>t is made to ensure that <strong>the</strong> list of providers on <strong>the</strong> BCBS Web site is up-to-date <strong>and</strong> accurate.<br />
However, <strong>the</strong> network is subject to change throughout <strong>the</strong> year. It is your responsibility to verify that <strong>the</strong> provider<br />
you or a covered family member uses is in <strong>the</strong> network associated with your health care option. You should call<br />
BCBS’s customer service department or access <strong>the</strong>ir Web site be<strong>for</strong>e you receive care to find out if a specific<br />
provider continues to be part of <strong>the</strong> network.<br />
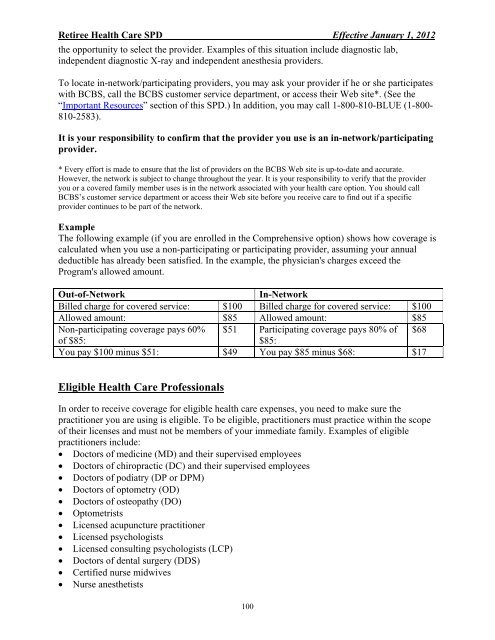
Example<br />
<strong>The</strong> following example (if you are enrolled in <strong>the</strong> Comprehensive option) shows how coverage is<br />
calculated when you use a non-participating or participating provider, assuming your annual<br />
deductible has already been satisfied. In <strong>the</strong> example, <strong>the</strong> physician's charges exceed <strong>the</strong><br />
Program's allowed amount.<br />
Out-of-Network In-Network<br />
Billed charge <strong>for</strong> covered service: $100 Billed charge <strong>for</strong> covered service: $100<br />
Allowed amount: $85 Allowed amount: $85<br />
Non-participating coverage pays 60% $51 Participating coverage pays 80% of $68<br />
of $85:<br />
$85:<br />
You pay $100 minus $51: $49 You pay $85 minus $68: $17<br />
Eligible Health Care Professionals<br />
In order to receive coverage <strong>for</strong> eligible health care expenses, you need to make sure <strong>the</strong><br />
practitioner you are using is eligible. To be eligible, practitioners must practice within <strong>the</strong> scope<br />
of <strong>the</strong>ir licenses <strong>and</strong> must not be members of your immediate family. Examples of eligible<br />
practitioners include:<br />
• Doctors of medicine (MD) <strong>and</strong> <strong>the</strong>ir supervised employees<br />
• Doctors of chiropractic (DC) <strong>and</strong> <strong>the</strong>ir supervised employees<br />
• Doctors of podiatry (DP or DPM)<br />
• Doctors of optometry (OD)<br />
• Doctors of osteopathy (DO)<br />
• Optometrists<br />
• Licensed acupuncture practitioner<br />
• Licensed psychologists<br />
• Licensed consulting psychologists (LCP)<br />
• Doctors of dental surgery (DDS)<br />
• Certified nurse midwives<br />
• Nurse anes<strong>the</strong>tists<br />
100