The eligibility and enrollment rules for the U
The eligibility and enrollment rules for the U
The eligibility and enrollment rules for the U
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
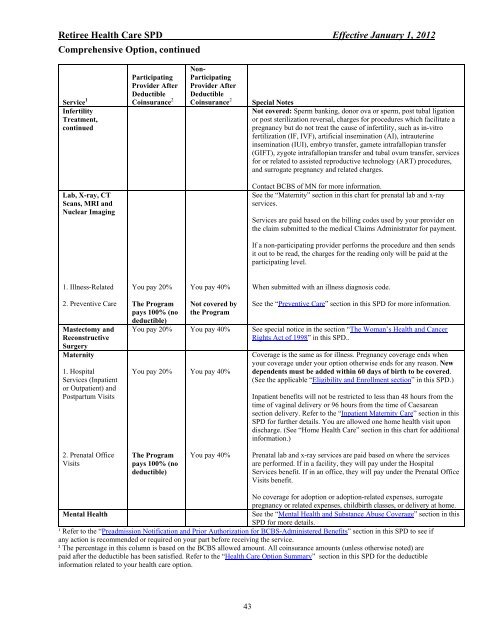
Retiree Health Care SPD Effective January 1, 2012<br />
Comprehensive Option, continued<br />
Service 1<br />
Infertility<br />
Treatment,<br />
continued<br />
Lab, X-ray, CT<br />
Scans, MRI <strong>and</strong><br />
Nuclear Imaging<br />
1. Illness-Related<br />
2. Preventive Care<br />
Mastectomy <strong>and</strong><br />
Reconstructive<br />
Surgery<br />
Maternity<br />
1. Hospital<br />
Services (Inpatient<br />
or Outpatient) <strong>and</strong><br />
Postpartum Visits<br />
2. Prenatal Office<br />
Visits<br />
Participating<br />
Provider After<br />
Deductible<br />
Coinsurance 2<br />
You pay 20%<br />
<strong>The</strong> Program<br />
pays 100% (no<br />
deductible)<br />
Non-<br />
Participating<br />
Provider After<br />
Deductible<br />
Coinsurance 2 Special Notes<br />
You pay 40%<br />
Not covered by<br />
<strong>the</strong> Program<br />
Not covered: Sperm banking, donor ova or sperm, post tubal ligation<br />
or post sterilization reversal, charges <strong>for</strong> procedures which facilitate a<br />
pregnancy but do not treat <strong>the</strong> cause of infertility, such as in-vitro<br />
fertilization (IF, IVF), artificial insemination (AI), intrauterine<br />
insemination (IUI), embryo transfer, gamete intrafallopian transfer<br />
(GIFT), zygote intrafallopian transfer <strong>and</strong> tubal ovum transfer, services<br />
<strong>for</strong> or related to assisted reproductive technology (ART) procedures,<br />
<strong>and</strong> surrogate pregnancy <strong>and</strong> related charges.<br />
Contact BCBS of MN <strong>for</strong> more in<strong>for</strong>mation.<br />
See <strong>the</strong> “Maternity” section in this chart <strong>for</strong> prenatal lab <strong>and</strong> x-ray<br />
services.<br />
Services are paid based on <strong>the</strong> billing codes used by your provider on<br />
<strong>the</strong> claim submitted to <strong>the</strong> medical Claims Administrator <strong>for</strong> payment.<br />
If a non-participating provider per<strong>for</strong>ms <strong>the</strong> procedure <strong>and</strong> <strong>the</strong>n sends<br />
it out to be read, <strong>the</strong> charges <strong>for</strong> <strong>the</strong> reading only will be paid at <strong>the</strong><br />
participating level.<br />
When submitted with an illness diagnosis code.<br />
See <strong>the</strong> “Preventive Care” section in this SPD <strong>for</strong> more in<strong>for</strong>mation.<br />
You pay 20% You pay 40% See special notice in <strong>the</strong> section “<strong>The</strong> Woman’s Health <strong>and</strong> Cancer<br />
Rights Act of 1998” in this SPD..<br />
You pay 20%<br />
<strong>The</strong> Program<br />
pays 100% (no<br />
deductible)<br />
You pay 40%<br />
You pay 40%<br />
Coverage is <strong>the</strong> same as <strong>for</strong> illness. Pregnancy coverage ends when<br />
your coverage under your option o<strong>the</strong>rwise ends <strong>for</strong> any reason. New<br />
dependents must be added within 60 days of birth to be covered.<br />
(See <strong>the</strong> applicable “Eligibility <strong>and</strong> Enrollment section” in this SPD.)<br />
Inpatient benefits will not be restricted to less than 48 hours from <strong>the</strong><br />
time of vaginal delivery or 96 hours from <strong>the</strong> time of Caesarean<br />
section delivery. Refer to <strong>the</strong> “Inpatient Maternity Care” section in this<br />
SPD <strong>for</strong> fur<strong>the</strong>r details. You are allowed one home health visit upon<br />
discharge. (See “Home Health Care” section in this chart <strong>for</strong> additional<br />
in<strong>for</strong>mation.)<br />
Prenatal lab <strong>and</strong> x-ray services are paid based on where <strong>the</strong> services<br />
are per<strong>for</strong>med. If in a facility, <strong>the</strong>y will pay under <strong>the</strong> Hospital<br />
Services benefit. If in an office, <strong>the</strong>y will pay under <strong>the</strong> Prenatal Office<br />
Visits benefit.<br />
No coverage <strong>for</strong> adoption or adoption-related expenses, surrogate<br />
pregnancy or related expenses, childbirth classes, or delivery at home.<br />
Mental Health See <strong>the</strong> “Mental Health <strong>and</strong> Substance Abuse Coverage” section in this<br />
SPD <strong>for</strong> more details.<br />
¹ Refer to <strong>the</strong> “Preadmission Notification <strong>and</strong> Prior Authorization <strong>for</strong> BCBS-Administered Benefits” section in this SPD to see if<br />
any action is recommended or required on your part be<strong>for</strong>e receiving <strong>the</strong> service.<br />
² <strong>The</strong> percentage in this column is based on <strong>the</strong> BCBS allowed amount. All coinsurance amounts (unless o<strong>the</strong>rwise noted) are<br />
paid after <strong>the</strong> deductible has been satisfied. Refer to <strong>the</strong> “Health Care Option Summary” section in this SPD <strong>for</strong> <strong>the</strong> deductible<br />
in<strong>for</strong>mation related to your health care option.<br />
43