The eligibility and enrollment rules for the U
The eligibility and enrollment rules for the U
The eligibility and enrollment rules for the U
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Retiree Health Care SPD Effective January 1, 2012<br />
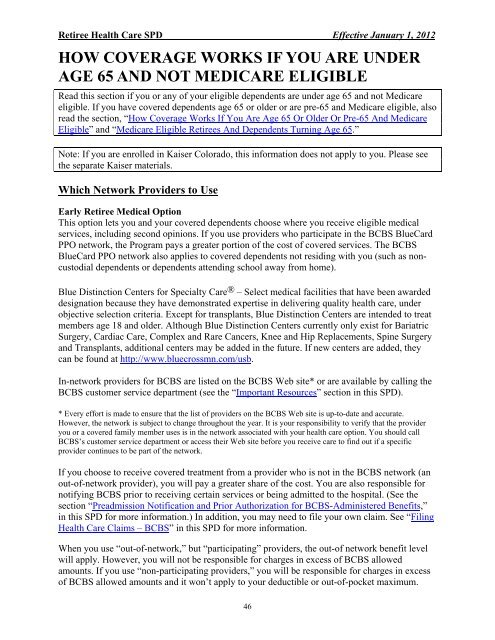
HOW COVERAGE WORKS IF YOU ARE UNDER<br />
AGE 65 AND NOT MEDICARE ELIGIBLE<br />
Read this section if you or any of your eligible dependents are under age 65 <strong>and</strong> not Medicare<br />
eligible. If you have covered dependents age 65 or older or are pre-65 <strong>and</strong> Medicare eligible, also<br />
read <strong>the</strong> section, “How Coverage Works If You Are Age 65 Or Older Or Pre-65 And Medicare<br />
Eligible” <strong>and</strong> “Medicare Eligible Retirees And Dependents Turning Age 65.”<br />
Note: If you are enrolled in Kaiser Colorado, this in<strong>for</strong>mation does not apply to you. Please see<br />
<strong>the</strong> separate Kaiser materials.<br />
Which Network Providers to Use<br />
Early Retiree Medical Option<br />
This option lets you <strong>and</strong> your covered dependents choose where you receive eligible medical<br />
services, including second opinions. If you use providers who participate in <strong>the</strong> BCBS BlueCard<br />
PPO network, <strong>the</strong> Program pays a greater portion of <strong>the</strong> cost of covered services. <strong>The</strong> BCBS<br />
BlueCard PPO network also applies to covered dependents not residing with you (such as noncustodial<br />
dependents or dependents attending school away from home).<br />
Blue Distinction Centers <strong>for</strong> Specialty Care ® – Select medical facilities that have been awarded<br />
designation because <strong>the</strong>y have demonstrated expertise in delivering quality health care, under<br />
objective selection criteria. Except <strong>for</strong> transplants, Blue Distinction Centers are intended to treat<br />
members age 18 <strong>and</strong> older. Although Blue Distinction Centers currently only exist <strong>for</strong> Bariatric<br />
Surgery, Cardiac Care, Complex <strong>and</strong> Rare Cancers, Knee <strong>and</strong> Hip Replacements, Spine Surgery<br />
<strong>and</strong> Transplants, additional centers may be added in <strong>the</strong> future. If new centers are added, <strong>the</strong>y<br />
can be found at http://www.bluecrossmn.com/usb.<br />
In-network providers <strong>for</strong> BCBS are listed on <strong>the</strong> BCBS Web site* or are available by calling <strong>the</strong><br />
BCBS customer service department (see <strong>the</strong> “Important Resources” section in this SPD).<br />
* Every ef<strong>for</strong>t is made to ensure that <strong>the</strong> list of providers on <strong>the</strong> BCBS Web site is up-to-date <strong>and</strong> accurate.<br />
However, <strong>the</strong> network is subject to change throughout <strong>the</strong> year. It is your responsibility to verify that <strong>the</strong> provider<br />
you or a covered family member uses is in <strong>the</strong> network associated with your health care option. You should call<br />
BCBS’s customer service department or access <strong>the</strong>ir Web site be<strong>for</strong>e you receive care to find out if a specific<br />
provider continues to be part of <strong>the</strong> network.<br />
If you choose to receive covered treatment from a provider who is not in <strong>the</strong> BCBS network (an<br />
out-of-network provider), you will pay a greater share of <strong>the</strong> cost. You are also responsible <strong>for</strong><br />
notifying BCBS prior to receiving certain services or being admitted to <strong>the</strong> hospital. (See <strong>the</strong><br />
section “Preadmission Notification <strong>and</strong> Prior Authorization <strong>for</strong> BCBS-Administered Benefits,”<br />
in this SPD <strong>for</strong> more in<strong>for</strong>mation.) In addition, you may need to file your own claim. See “Filing<br />
Health Care Claims – BCBS” in this SPD <strong>for</strong> more in<strong>for</strong>mation.<br />
When you use “out-of-network,” but “participating” providers, <strong>the</strong> out-of network benefit level<br />
will apply. However, you will not be responsible <strong>for</strong> charges in excess of BCBS allowed<br />
amounts. If you use “non-participating providers,” you will be responsible <strong>for</strong> charges in excess<br />
of BCBS allowed amounts <strong>and</strong> it won’t apply to your deductible or out-of-pocket maximum.<br />
46