The eligibility and enrollment rules for the U
The eligibility and enrollment rules for the U
The eligibility and enrollment rules for the U
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
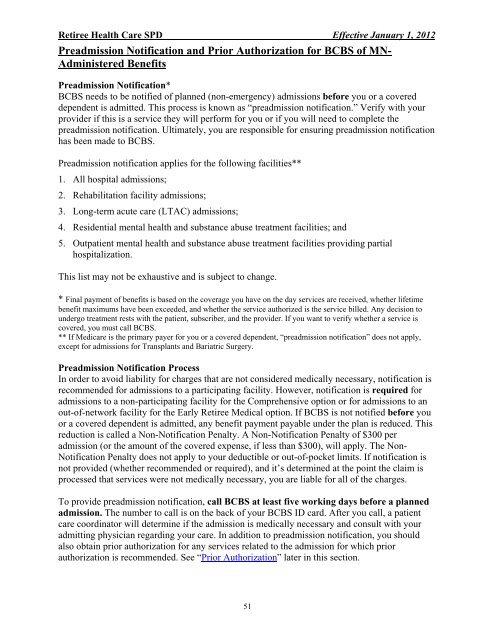
Retiree Health Care SPD Effective January 1, 2012<br />
Preadmission Notification <strong>and</strong> Prior Authorization <strong>for</strong> BCBS of MN-<br />
Administered Benefits<br />
Preadmission Notification*<br />
BCBS needs to be notified of planned (non-emergency) admissions be<strong>for</strong>e you or a covered<br />
dependent is admitted. This process is known as “preadmission notification.” Verify with your<br />
provider if this is a service <strong>the</strong>y will per<strong>for</strong>m <strong>for</strong> you or if you will need to complete <strong>the</strong><br />
preadmission notification. Ultimately, you are responsible <strong>for</strong> ensuring preadmission notification<br />
has been made to BCBS.<br />
Preadmission notification applies <strong>for</strong> <strong>the</strong> following facilities**<br />
1. All hospital admissions;<br />
2. Rehabilitation facility admissions;<br />
3. Long-term acute care (LTAC) admissions;<br />
4. Residential mental health <strong>and</strong> substance abuse treatment facilities; <strong>and</strong><br />
5. Outpatient mental health <strong>and</strong> substance abuse treatment facilities providing partial<br />
hospitalization.<br />
This list may not be exhaustive <strong>and</strong> is subject to change.<br />
* Final payment of benefits is based on <strong>the</strong> coverage you have on <strong>the</strong> day services are received, whe<strong>the</strong>r lifetime<br />
benefit maximums have been exceeded, <strong>and</strong> whe<strong>the</strong>r <strong>the</strong> service authorized is <strong>the</strong> service billed. Any decision to<br />
undergo treatment rests with <strong>the</strong> patient, subscriber, <strong>and</strong> <strong>the</strong> provider. If you want to verify whe<strong>the</strong>r a service is<br />
covered, you must call BCBS.<br />
** If Medicare is <strong>the</strong> primary payer <strong>for</strong> you or a covered dependent, “preadmission notification” does not apply,<br />
except <strong>for</strong> admissions <strong>for</strong> Transplants <strong>and</strong> Bariatric Surgery.<br />
Preadmission Notification Process<br />
In order to avoid liability <strong>for</strong> charges that are not considered medically necessary, notification is<br />
recommended <strong>for</strong> admissions to a participating facility. However, notification is required <strong>for</strong><br />
admissions to a non-participating facility <strong>for</strong> <strong>the</strong> Comprehensive option or <strong>for</strong> admissions to an<br />
out-of-network facility <strong>for</strong> <strong>the</strong> Early Retiree Medical option. If BCBS is not notified be<strong>for</strong>e you<br />
or a covered dependent is admitted, any benefit payment payable under <strong>the</strong> plan is reduced. This<br />
reduction is called a Non-Notification Penalty. A Non-Notification Penalty of $300 per<br />
admission (or <strong>the</strong> amount of <strong>the</strong> covered expense, if less than $300), will apply. <strong>The</strong> Non-<br />
Notification Penalty does not apply to your deductible or out-of-pocket limits. If notification is<br />
not provided (whe<strong>the</strong>r recommended or required), <strong>and</strong> it’s determined at <strong>the</strong> point <strong>the</strong> claim is<br />
processed that services were not medically necessary, you are liable <strong>for</strong> all of <strong>the</strong> charges.<br />
To provide preadmission notification, call BCBS at least five working days be<strong>for</strong>e a planned<br />
admission. <strong>The</strong> number to call is on <strong>the</strong> back of your BCBS ID card. After you call, a patient<br />
care coordinator will determine if <strong>the</strong> admission is medically necessary <strong>and</strong> consult with your<br />
admitting physician regarding your care. In addition to preadmission notification, you should<br />
also obtain prior authorization <strong>for</strong> any services related to <strong>the</strong> admission <strong>for</strong> which prior<br />
authorization is recommended. See “Prior Authorization” later in this section.<br />
51