The eligibility and enrollment rules for the U
The eligibility and enrollment rules for the U
The eligibility and enrollment rules for the U
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
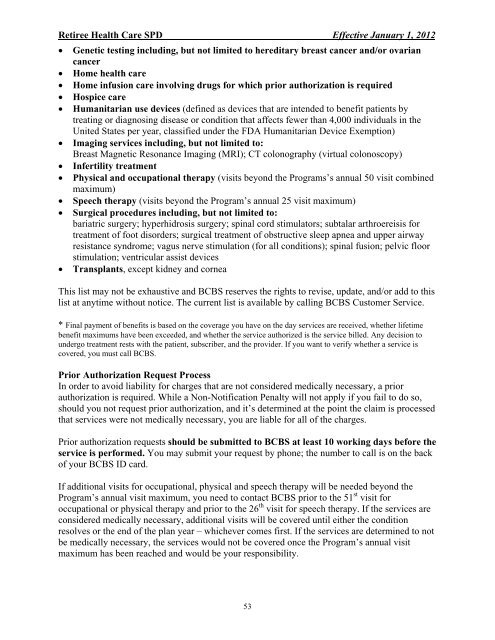
Retiree Health Care SPD Effective January 1, 2012<br />
• Genetic testing including, but not limited to hereditary breast cancer <strong>and</strong>/or ovarian<br />
cancer<br />
• Home health care<br />
• Home infusion care involving drugs <strong>for</strong> which prior authorization is required<br />
• Hospice care<br />
• Humanitarian use devices (defined as devices that are intended to benefit patients by<br />
treating or diagnosing disease or condition that affects fewer than 4,000 individuals in <strong>the</strong><br />
United States per year, classified under <strong>the</strong> FDA Humanitarian Device Exemption)<br />
• Imaging services including, but not limited to:<br />
Breast Magnetic Resonance Imaging (MRI); CT colonography (virtual colonoscopy)<br />
• Infertility treatment<br />
• Physical <strong>and</strong> occupational <strong>the</strong>rapy (visits beyond <strong>the</strong> Programs’s annual 50 visit combined<br />
maximum)<br />
• Speech <strong>the</strong>rapy (visits beyond <strong>the</strong> Program’s annual 25 visit maximum)<br />
• Surgical procedures including, but not limited to:<br />
bariatric surgery; hyperhidrosis surgery; spinal cord stimulators; subtalar arthroereisis <strong>for</strong><br />
treatment of foot disorders; surgical treatment of obstructive sleep apnea <strong>and</strong> upper airway<br />
resistance syndrome; vagus nerve stimulation (<strong>for</strong> all conditions); spinal fusion; pelvic floor<br />
stimulation; ventricular assist devices<br />
• Transplants, except kidney <strong>and</strong> cornea<br />
This list may not be exhaustive <strong>and</strong> BCBS reserves <strong>the</strong> rights to revise, update, <strong>and</strong>/or add to this<br />
list at anytime without notice. <strong>The</strong> current list is available by calling BCBS Customer Service.<br />
* Final payment of benefits is based on <strong>the</strong> coverage you have on <strong>the</strong> day services are received, whe<strong>the</strong>r lifetime<br />
benefit maximums have been exceeded, <strong>and</strong> whe<strong>the</strong>r <strong>the</strong> service authorized is <strong>the</strong> service billed. Any decision to<br />
undergo treatment rests with <strong>the</strong> patient, subscriber, <strong>and</strong> <strong>the</strong> provider. If you want to verify whe<strong>the</strong>r a service is<br />
covered, you must call BCBS.<br />
Prior Authorization Request Process<br />
In order to avoid liability <strong>for</strong> charges that are not considered medically necessary, a prior<br />
authorization is required. While a Non-Notification Penalty will not apply if you fail to do so,<br />
should you not request prior authorization, <strong>and</strong> it’s determined at <strong>the</strong> point <strong>the</strong> claim is processed<br />
that services were not medically necessary, you are liable <strong>for</strong> all of <strong>the</strong> charges.<br />
Prior authorization requests should be submitted to BCBS at least 10 working days be<strong>for</strong>e <strong>the</strong><br />
service is per<strong>for</strong>med. You may submit your request by phone; <strong>the</strong> number to call is on <strong>the</strong> back<br />
of your BCBS ID card.<br />
If additional visits <strong>for</strong> occupational, physical <strong>and</strong> speech <strong>the</strong>rapy will be needed beyond <strong>the</strong><br />
Program’s annual visit maximum, you need to contact BCBS prior to <strong>the</strong> 51 st visit <strong>for</strong><br />
occupational or physical <strong>the</strong>rapy <strong>and</strong> prior to <strong>the</strong> 26 th visit <strong>for</strong> speech <strong>the</strong>rapy. If <strong>the</strong> services are<br />
considered medically necessary, additional visits will be covered until ei<strong>the</strong>r <strong>the</strong> condition<br />
resolves or <strong>the</strong> end of <strong>the</strong> plan year – whichever comes first. If <strong>the</strong> services are determined to not<br />
be medically necessary, <strong>the</strong> services would not be covered once <strong>the</strong> Program’s annual visit<br />
maximum has been reached <strong>and</strong> would be your responsibility.<br />
53