The eligibility and enrollment rules for the U
The eligibility and enrollment rules for the U
The eligibility and enrollment rules for the U
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Retiree Health Care SPD Effective January 1, 2012<br />
For BCBS participants using a non-participating provider, if <strong>the</strong> provider is:<br />
• a facility in Minnesota, <strong>the</strong> allowed amount is a designated percentage of <strong>the</strong> facility’s billed<br />
charges. Outside of Minnesota, <strong>the</strong> allowed amount is determined by <strong>the</strong> local Blue Cross<br />
<strong>and</strong>/or Blue Shield Plan, unless that amount is greater than <strong>the</strong> billed charge, or no allowed<br />
amount is provided by <strong>the</strong> local Blue Plan. In that case, <strong>the</strong> allowed amount is determined<br />
from a Medicare-based fee schedule. If such pricing is not available, payment will be based<br />
on a percentage of <strong>the</strong> billed charges.<br />
• a physician or clinic in Minnesota, <strong>the</strong> allowed amount is <strong>the</strong> lesser of: (1) <strong>the</strong><br />
Nonparticipating Provider Professional Services in Minnesota Fee Schedule or (2) a<br />
designated percentage of <strong>the</strong> billed charges. Outside of Minnesota, <strong>the</strong> allowed amount is<br />
determined by <strong>the</strong> local Blue Cross <strong>and</strong>/or Blue Shield Plan, unless that amount is greater<br />
than <strong>the</strong> billed charge, or no allowed amount is provided by <strong>the</strong> local Blue Plan. In that case,<br />
<strong>the</strong> allowed amount payment will be based on a percentage of pricing obtained from a<br />
nationwide provider reimbursement database that considers various factors, including <strong>the</strong> zip<br />
code of <strong>the</strong> place of service <strong>and</strong> <strong>the</strong> type of service provided. If this database pricing is not<br />
available <strong>for</strong> <strong>the</strong> service provided, payment will be based on <strong>the</strong> lesser of: (1) <strong>the</strong><br />
Nonparticipating Provider Professional Services in Minnesota Fee Schedule or (2) a<br />
designated percentage of <strong>the</strong> billed charges.<br />
When you receive care from certain non-participating professionals, <strong>the</strong> reimbursement to <strong>the</strong><br />
non-participating professional may include some of <strong>the</strong> costs that you would o<strong>the</strong>rwise be<br />
required to pay (e.g., <strong>the</strong> difference between <strong>the</strong> allowed amount <strong>and</strong> <strong>the</strong> provider's billed charge)<br />
as well as <strong>the</strong> services may be paid at <strong>the</strong> highest level of benefits. This applies in limited<br />
circumstances when you receive care from non-participating professionals <strong>and</strong> you did not have<br />
<strong>the</strong> opportunity to select <strong>the</strong> provider. Examples of this situation include diagnostic lab,<br />
independent diagnostic X-ray <strong>and</strong> independent anes<strong>the</strong>sia providers.<br />
To locate in-network/participating providers, call <strong>the</strong> BCBS customer service department or<br />
access <strong>the</strong>ir Web site*. (See <strong>the</strong> “Important Resources” section in this SPD.) It is your<br />
responsibility to confirm that <strong>the</strong> provider you use is an in-network/participating provider.<br />
* Every ef<strong>for</strong>t is made to ensure that <strong>the</strong> list of providers on <strong>the</strong> BCBS Web site is up-to-date <strong>and</strong> accurate.<br />
However, <strong>the</strong> network is subject to change throughout <strong>the</strong> year. It is your responsibility to verify that <strong>the</strong> provider<br />
you or a covered family member uses is in <strong>the</strong> network associated with your health care option. You should call<br />
BCBS’s customer service department or access <strong>the</strong>ir Web site be<strong>for</strong>e you receive care to find out if a specific<br />
provider continues to be part of <strong>the</strong> network.<br />
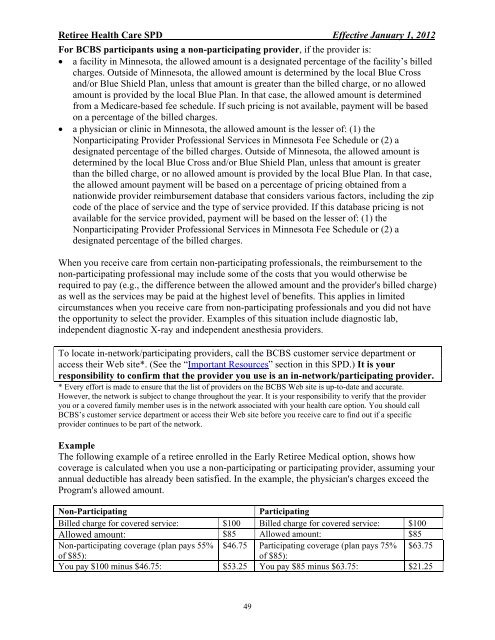
Example<br />
<strong>The</strong> following example of a retiree enrolled in <strong>the</strong> Early Retiree Medical option, shows how<br />
coverage is calculated when you use a non-participating or participating provider, assuming your<br />
annual deductible has already been satisfied. In <strong>the</strong> example, <strong>the</strong> physician's charges exceed <strong>the</strong><br />
Program's allowed amount.<br />
Non-Participating Participating<br />
Billed charge <strong>for</strong> covered service: $100 Billed charge <strong>for</strong> covered service: $100<br />
Allowed amount: $85 Allowed amount: $85<br />
Non-participating coverage (plan pays 55% $46.75 Participating coverage (plan pays 75% $63.75<br />
of $85):<br />
of $85):<br />
You pay $100 minus $46.75: $53.25 You pay $85 minus $63.75: $21.25<br />
49