Indiana State Health Improvement Plan (I-SHIP) - State of Indiana
Indiana State Health Improvement Plan (I-SHIP) - State of Indiana
Indiana State Health Improvement Plan (I-SHIP) - State of Indiana
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
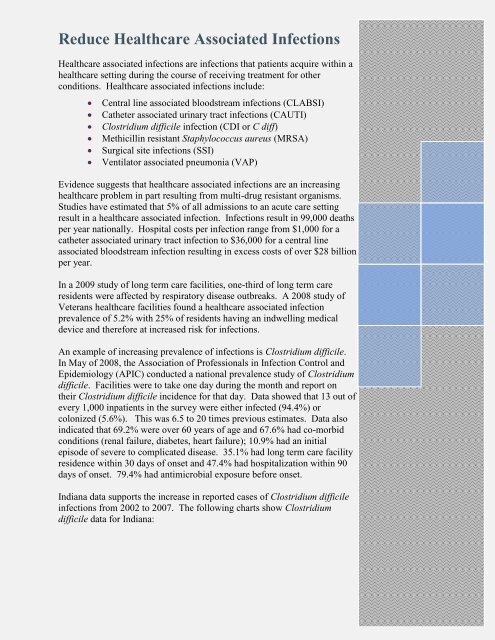
Reduce <strong>Health</strong>care Associated Infections<br />
<strong>Health</strong>care associated infections are infections that patients acquire within a<br />
healthcare setting during the course <strong>of</strong> receiving treatment for other<br />
conditions. <strong>Health</strong>care associated infections include:<br />
� Central line associated bloodstream infections (CLABSI)<br />
� Catheter associated urinary tract infections (CAUTI)<br />
� Clostridium difficile infection (CDI or C diff)<br />
� Methicillin resistant Staphylococcus aureus (MRSA)<br />
� Surgical site infections (SSI)<br />
� Ventilator associated pneumonia (VAP)<br />
Evidence suggests that healthcare associated infections are an increasing<br />
healthcare problem in part resulting from multi-drug resistant organisms.<br />
Studies have estimated that 5% <strong>of</strong> all admissions to an acute care setting<br />
result in a healthcare associated infection. Infections result in 99,000 deaths<br />
per year nationally. Hospital costs per infection range from $1,000 for a<br />
catheter associated urinary tract infection to $36,000 for a central line<br />
associated bloodstream infection resulting in excess costs <strong>of</strong> over $28 billion<br />
per year.<br />
In a 2009 study <strong>of</strong> long term care facilities, one-third <strong>of</strong> long term care<br />
residents were affected by respiratory disease outbreaks. A 2008 study <strong>of</strong><br />
Veterans healthcare facilities found a healthcare associated infection<br />
prevalence <strong>of</strong> 5.2% with 25% <strong>of</strong> residents having an indwelling medical<br />
device and therefore at increased risk for infections.<br />
An example <strong>of</strong> increasing prevalence <strong>of</strong> infections is Clostridium difficile.<br />
In May <strong>of</strong> 2008, the Association <strong>of</strong> Pr<strong>of</strong>essionals in Infection Control and<br />
Epidemiology (APIC) conducted a national prevalence study <strong>of</strong> Clostridium<br />
difficile. Facilities were to take one day during the month and report on<br />
their Clostridium difficile incidence for that day. Data showed that 13 out <strong>of</strong><br />
every 1,000 inpatients in the survey were either infected (94.4%) or<br />
colonized (5.6%). This was 6.5 to 20 times previous estimates. Data also<br />
indicated that 69.2% were over 60 years <strong>of</strong> age and 67.6% had co-morbid<br />
conditions (renal failure, diabetes, heart failure); 10.9% had an initial<br />
episode <strong>of</strong> severe to complicated disease. 35.1% had long term care facility<br />
residence within 30 days <strong>of</strong> onset and 47.4% had hospitalization within 90<br />
days <strong>of</strong> onset. 79.4% had antimicrobial exposure before onset.<br />
<strong>Indiana</strong> data supports the increase in reported cases <strong>of</strong> Clostridium difficile<br />
infections from 2002 to 2007. The following charts show Clostridium<br />
difficile data for <strong>Indiana</strong>: