Pathology of the Head and Neck
Pathology of the Head and Neck
Pathology of the Head and Neck
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
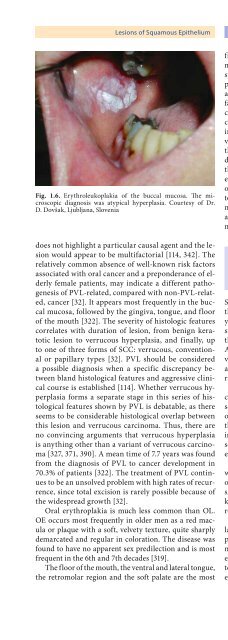
Lesions <strong>of</strong> Squamous Epi<strong>the</strong>lium Chapter 1 7Fig. 1.6. Erythroleukoplakia <strong>of</strong> <strong>the</strong> buccal mucosa. The microscopicdiagnosis was atypical hyperplasia. Courtesy <strong>of</strong> Dr.D. Dovšak, Ljubljana, Sloveniadoes not highlight a particular causal agent <strong>and</strong> <strong>the</strong> lesionwould appear to be multifactorial [114, 342]. Therelatively common absence <strong>of</strong> well-known risk factorsassociated with oral cancer <strong>and</strong> a preponderance <strong>of</strong> elderlyfemale patients, may indicate a different pathogenesis<strong>of</strong> PVL-related, compared with non-PVL-related,cancer [32]. It appears most frequently in <strong>the</strong> buccalmucosa, followed by <strong>the</strong> gingiva, tongue, <strong>and</strong> floor<strong>of</strong> <strong>the</strong> mouth [322]. The severity <strong>of</strong> histologic featurescorrelates with duration <strong>of</strong> lesion, from benign keratoticlesion to verrucous hyperplasia, <strong>and</strong> finally, upto one <strong>of</strong> three forms <strong>of</strong> SCC: verrucous, conventionalor papillary types [32]. PVL should be considereda possible diagnosis when a specific discrepancy betweenbl<strong>and</strong> histological features <strong>and</strong> aggressive clinicalcourse is established [114]. Whe<strong>the</strong>r verrucous hyperplasiaforms a separate stage in this series <strong>of</strong> histologicalfeatures shown by PVL is debatable, as <strong>the</strong>reseems to be considerable histological overlap betweenthis lesion <strong>and</strong> verrucous carcinoma. Thus, <strong>the</strong>re areno convincing arguments that verrucous hyperplasiais anything o<strong>the</strong>r than a variant <strong>of</strong> verrucous carcinoma[327, 371, 390]. A mean time <strong>of</strong> 7.7 years was foundfrom <strong>the</strong> diagnosis <strong>of</strong> PVL to cancer development in70.3% <strong>of</strong> patients [322]. The treatment <strong>of</strong> PVL continuesto be an unsolved problem with high rates <strong>of</strong> recurrence,since total excision is rarely possible because <strong>of</strong><strong>the</strong> widespread growth [32].Oral erythroplakia is much less common than OL.OE occurs most frequently in older men as a red maculaor plaque with a s<strong>of</strong>t, velvety texture, quite sharplydemarcated <strong>and</strong> regular in coloration. The disease wasfound to have no apparent sex predilection <strong>and</strong> is mostfrequent in <strong>the</strong> 6th <strong>and</strong> 7th decades [319].The floor <strong>of</strong> <strong>the</strong> mouth, <strong>the</strong> ventral <strong>and</strong> lateral tongue,<strong>the</strong> retromolar region <strong>and</strong> <strong>the</strong> s<strong>of</strong>t palate are <strong>the</strong> mostfrequently involved sites [47, 263]. OEs that are intermixedwith white areas are called erythroleukoplakia orspeckled mucosa <strong>and</strong> are believed to behave similarly topure OE. The red appearance <strong>of</strong> OE may be related toan increase in subepi<strong>the</strong>lial blood vessels, a lack <strong>of</strong> surfacekeratin <strong>and</strong> thinness <strong>of</strong> <strong>the</strong> epi<strong>the</strong>lium. Prior to aclinical diagnosis <strong>of</strong> OE numerous entities should be excluded,such as: median rhomboid glossitis, all kinds <strong>of</strong>injuries, infectious <strong>and</strong> allergic lesions, haemorrhages,vessel tumours, Wegener’s granulomatosis, etc. [47]. AlthoughOE is a rare lesion, it is much more likely to showdysplasia or carcinoma. Shafer <strong>and</strong> Waldron reviewed<strong>the</strong>ir biopsy experiences with 65 cases <strong>of</strong> OE: 51% <strong>of</strong> casesshowed invasive SCC, 40% were carcinomas in situor severe dysplasia, <strong>and</strong> <strong>the</strong> remaining 9% showed mildto moderate dysplasia [319]. In all red lesions <strong>of</strong> <strong>the</strong> oralmucosa that do not regress within 2 weeks <strong>of</strong> <strong>the</strong> removal<strong>of</strong> possible aetiological factors, biopsy is, <strong>the</strong>refore,m<strong>and</strong>atory.1.2.4.2 Laryngeal<strong>and</strong> HypopharyngealLeukoplakia <strong>and</strong>Chronic LaryngitisSquamous intraepi<strong>the</strong>lial lesions appear mainly along<strong>the</strong> true vocal cords, <strong>and</strong> rarely in o<strong>the</strong>r parts <strong>of</strong> <strong>the</strong> larynx,such as <strong>the</strong> epiglottis. Two-thirds <strong>of</strong> vocal cord lesionsare bilateral [48, 178, 181]. They can extend over<strong>the</strong> free edge <strong>of</strong> <strong>the</strong> vocal cord to its subglottic surface.An origin in, or extension along <strong>the</strong> upper surface <strong>of</strong> <strong>the</strong>vocal cord is less common [181, 194]. The commissuresare rarely involved [48]. Hypopharyngeal lesions arerarely found <strong>and</strong> are poorly defined [364].Laryngeal SILs do not have a single distinctive orcharacteristic clinical appearance <strong>and</strong> are variously describedas leukoplakia, chronic hyperplastic laryngitisor rarely erythroplakia. A circumscribed thickening <strong>of</strong><strong>the</strong> mucosa covered by whitish patches (Fig. 1.7), or anirregularly growing, well-defined warty plaque may beseen. A speckled appearance <strong>of</strong> lesions can also be present,caused by unequal thickness <strong>of</strong> <strong>the</strong> keratin layer.However, <strong>the</strong> lesions are commonly more diffuse,with a thickened appearance, <strong>and</strong> occupy a large part <strong>of</strong>one or both vocal cords (Fig. 1.8). A few leukoplakic lesionsare ulcerated (6.5%) or combined with erythroplakia(15%) [48]. Leukoplakic lesions, in contrast to erythroplakicones, tend to be well demarcated.The macroscopic features <strong>of</strong> hypopharyngeal <strong>and</strong>laryngeal SILs are not as well defined as <strong>the</strong>ir counterpartsin <strong>the</strong> oral cavity <strong>and</strong> <strong>the</strong>ir relative importance isnot generally accepted. Most patients with SILs presentwith a history <strong>of</strong> a few months or more <strong>of</strong> symptoms;an average duration <strong>of</strong> 7 months has been reported[48]. Symptoms depend on <strong>the</strong> location <strong>and</strong> sever-