Global Tuberculosis Report -- 2012.pdf
Global Tuberculosis Report -- 2012.pdf
Global Tuberculosis Report -- 2012.pdf
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
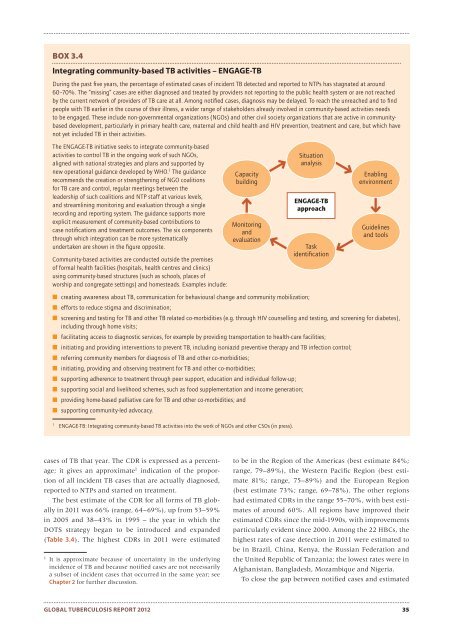
BOX 3.4Integrating community-based TB activities – ENGAGE-TBDuring the past fi ve years, the percentage of estimated cases of incident TB detected and reported to NTPs has stagnated at around60–70%. The “missing” cases are either diagnosed and treated by providers not reporting to the public health system or are not reachedby the current network of providers of TB care at all. Among notifi ed cases, diagnosis may be delayed. To reach the unreached and to fi ndpeople with TB earlier in the course of their illness, a wider range of stakeholders already involved in community-based activities needsto be engaged. These include non-governmental organizations (NGOs) and other civil society organizations that are active in communitybaseddevelopment, particularly in primary health care, maternal and child health and HIV prevention, treatment and care, but which havenot yet included TB in their activities.The ENGAGE-TB initiative seeks to integrate community-basedactivities to control TB in the ongoing work of such NGOs,aligned with national strategies and plans and supported bynew operational guidance developed by WHO. 1 The guidancerecommends the creation or strengthening of NGO coalitionsfor TB care and control, regular meetings between theleadership of such coalitions and NTP staff at various levels,and streamlining monitoring and evaluation through a singlerecording and reporting system. The guidance supports moreexplicit measurement of community-based contributions tocase notifi cations and treatment outcomes. The six componentsthrough which integration can be more systematicallyundertaken are shown in the fi gure opposite.Community-based activities are conducted outside the premisesof formal health facilities (hospitals, health centres and clinics)using community-based structures (such as schools, places ofworship and congregate settings) and homesteads. Examples include:CapacitybuildingMonitoringandevaluation■ creating awareness about TB, communication for behavioural change and community mobilization;■ efforts to reduce stigma and discrimination;■ screening and testing for TB and other TB related co-morbidities (e.g. through HIV counselling and testing, and screening for diabetes),including through home visits;■ facilitating access to diagnostic services, for example by providing transportation to health-care facilities;■ initiating and providing interventions to prevent TB, including isoniazid preventive therapy and TB infection control;■ referring community members for diagnosis of TB and other co-morbidities;■ initiating, providing and observing treatment for TB and other co-morbidities;■ supporting adherence to treatment through peer support, education and individual follow-up;■ supporting social and livelihood schemes, such as food supplementation and income generation;■ providing home-based palliative care for TB and other co-morbidities; and■ supporting community-led advocacy.1ENGAGE-TB: Integrating community-based TB activities into the work of NGOs and other CSOs (in press).SituationanalysisENGAGE-TBapproachTaskidentifi cationEnablingenvironmentGuidelinesand toolscases of TB that year. The CDR is expressed as a percentage;it gives an approximate 1 indication of the proportionof all incident TB cases that are actually diagnosed,reported to NTPs and started on treatment.The best estimate of the CDR for all forms of TB globallyin 2011 was 66% (range, 64–69%), up from 53–59%in 2005 and 38–43% in 1995 – the year in which theDOTS strategy began to be introduced and expanded(Table 3.4). The highest CDRs in 2011 were estimated1It is approximate because of uncertainty in the underlyingincidence of TB and because notified cases are not necessarilya subset of incident cases that occurred in the same year; seeChapter 2 for further discussion.to be in the Region of the Americas (best estimate 84%;range, 79–89%), the Western Pacific Region (best estimate81%; range, 75–89%) and the European Region(best estimate 73%; range, 69–78%). The other regionshad estimated CDRs in the range 55–70%, with best estimatesof around 60%. All regions have improved theirestimated CDRs since the mid-1990s, with improvementsparticularly evident since 2000. Among the 22 HBCs, thehighest rates of case detection in 2011 were estimated tobe in Brazil, China, Kenya, the Russian Federation andthe United Republic of Tanzania; the lowest rates were inAfghanistan, Bangladesh, Mozambique and Nigeria.To close the gap between notified cases and estimatedGLOBAL TUBERCULOSIS REPORT 2012 35