equity implications of health sector user fees in tanzania
equity implications of health sector user fees in tanzania
equity implications of health sector user fees in tanzania
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
II LITERATURE REVIEW<br />
2.1 Introduction to the overall <strong>user</strong> fee debate<br />
Background<br />
The <strong>user</strong> fee debate is full <strong>of</strong> controversies. The alleged positive and negative impacts <strong>of</strong> <strong>user</strong> <strong>fees</strong> on<br />
efficiency, <strong>equity</strong>, quality and susta<strong>in</strong>ability have led to heated debates among <strong>health</strong> <strong>sector</strong><br />
stakeholders. Almost without exception, the donor community strongly supported the cost-shar<strong>in</strong>g<br />
approach to education and <strong>health</strong> progressively <strong>in</strong>troduced <strong>in</strong> the 1980s and 1990s. The IMF and WB<br />
have traditionally promoted <strong>user</strong> <strong>fees</strong>, although their <strong>of</strong>ficial policy is more careful nowadays. They<br />
considered charges at the po<strong>in</strong>t <strong>of</strong> use needed to deter frivolous use and to help br<strong>in</strong>g money <strong>in</strong>to<br />
cash-strapped <strong>health</strong> systems (Rowson, 2004). Toward the late 1990s, however, other donors started<br />
to change their position regard<strong>in</strong>g the desirability <strong>of</strong> <strong>user</strong> <strong>fees</strong>. This trend is confirmed by Bennet and<br />
Gilson (2001) and the WHO World Health Report 2000. They conclude that “the focus <strong>of</strong> the<br />
<strong>in</strong>ternational debate is on the need to move away from excessive reliance on out-<strong>of</strong>-pocket payment<br />
as a source <strong>of</strong> <strong>health</strong> f<strong>in</strong>anc<strong>in</strong>g towards a system which <strong>in</strong>corporates a greater element <strong>of</strong> risk pool<strong>in</strong>g<br />
(for example, through <strong>health</strong> <strong>in</strong>surance) and thus affords greater protection for the poor.<br />
Commonly used systems<br />
Health care systems, particularly those <strong>in</strong> develop<strong>in</strong>g countries, typically depend on a mix <strong>of</strong> f<strong>in</strong>anc<strong>in</strong>g<br />
mechanisms rather than only one. The pr<strong>in</strong>cipal mechanisms are: (1) tax-based f<strong>in</strong>anc<strong>in</strong>g, (2) social<br />
<strong>in</strong>surance f<strong>in</strong>anc<strong>in</strong>g, (3) private <strong>in</strong>surance, (4) <strong>user</strong> <strong>fees</strong> and (5) community-based <strong>health</strong> <strong>in</strong>surance. It<br />
is common for different population segments to be covered by different types <strong>of</strong> f<strong>in</strong>anc<strong>in</strong>g mechanism.<br />
The degree to which the f<strong>in</strong>anc<strong>in</strong>g system as a whole is pro-poor depends on how the different<br />
mechanisms <strong>in</strong>teract (Bennet & Gilson, 2001). Two broad models <strong>of</strong> <strong>user</strong> fee systems have been<br />
adopted <strong>in</strong> African countries: (1) the ‘standard model’ and (2) the ‘Bamako Initiative model’ (Nolan and<br />
Turbat, 1995; <strong>in</strong> Gilson, 1997) (See Technical Paper Part 1). There is a wide range <strong>of</strong> different types<br />
<strong>of</strong> <strong>user</strong> fee payment systems: flat fee or differentiated fee; fee per episode or fee per item <strong>of</strong> service;<br />
prepayment or payment at time <strong>of</strong> use (Price, 2002). In addition to formal <strong>user</strong> <strong>fees</strong>, <strong>in</strong>formal charges<br />
are common practice (Nyonator and Kutz<strong>in</strong>, 1999).<br />
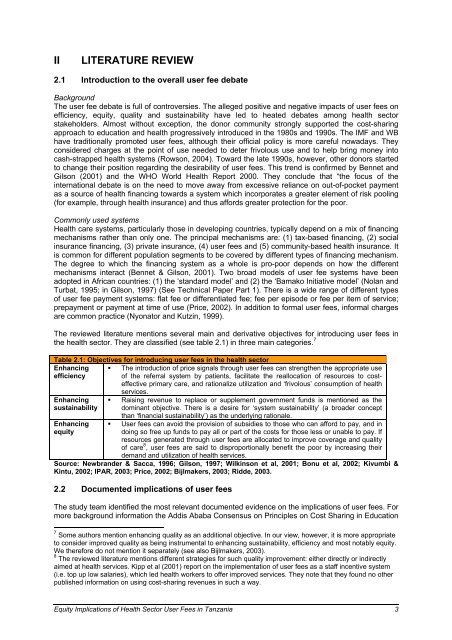
The reviewed literature mentions several ma<strong>in</strong> and derivative objectives for <strong>in</strong>troduc<strong>in</strong>g <strong>user</strong> <strong>fees</strong> <strong>in</strong><br />
the <strong>health</strong> <strong>sector</strong>. They are classified (see table 2.1) <strong>in</strong> three ma<strong>in</strong> categories. 7<br />
Table 2.1: Objectives for <strong>in</strong>troduc<strong>in</strong>g <strong>user</strong> <strong>fees</strong> <strong>in</strong> the <strong>health</strong> <strong>sector</strong><br />
Enhanc<strong>in</strong>g<br />
efficiency<br />
Enhanc<strong>in</strong>g<br />
susta<strong>in</strong>ability<br />
Enhanc<strong>in</strong>g<br />
<strong>equity</strong><br />
� The <strong>in</strong>troduction <strong>of</strong> price signals through <strong>user</strong> <strong>fees</strong> can strengthen the appropriate use<br />
<strong>of</strong> the referral system by patients, facilitate the reallocation <strong>of</strong> resources to costeffective<br />
primary care, and rationalize utilization and ‘frivolous’ consumption <strong>of</strong> <strong>health</strong><br />
services.<br />
� Rais<strong>in</strong>g revenue to replace or supplement government funds is mentioned as the<br />
dom<strong>in</strong>ant objective. There is a desire for ‘system susta<strong>in</strong>ability’ (a broader concept<br />
than ‘f<strong>in</strong>ancial susta<strong>in</strong>ability’) as the underly<strong>in</strong>g rationale.<br />
� User <strong>fees</strong> can avoid the provision <strong>of</strong> subsidies to those who can afford to pay, and <strong>in</strong><br />
do<strong>in</strong>g so free up funds to pay all or part <strong>of</strong> the costs for those less or unable to pay. If<br />
resources generated through <strong>user</strong> <strong>fees</strong> are allocated to improve coverage and quality<br />
<strong>of</strong> care 8 , <strong>user</strong> <strong>fees</strong> are said to disproportionally benefit the poor by <strong>in</strong>creas<strong>in</strong>g their<br />
demand and utilization <strong>of</strong> <strong>health</strong> services.<br />
Source: Newbrander & Sacca, 1996; Gilson, 1997; Wilk<strong>in</strong>son et al, 2001; Bonu et al, 2002; Kivumbi &<br />
K<strong>in</strong>tu, 2002; IPAR, 2003; Price, 2002; Bijlmakers, 2003; Ridde, 2003.<br />
2.2 Documented <strong>implications</strong> <strong>of</strong> <strong>user</strong> <strong>fees</strong><br />
The study team identified the most relevant documented evidence on the <strong>implications</strong> <strong>of</strong> <strong>user</strong> <strong>fees</strong>. For<br />
more background <strong>in</strong>formation the Addis Ababa Consensus on Pr<strong>in</strong>ciples on Cost Shar<strong>in</strong>g <strong>in</strong> Education<br />
7 Some authors mention enhanc<strong>in</strong>g quality as an additional objective. In our view, however, it is more appropriate<br />
to consider improved quality as be<strong>in</strong>g <strong>in</strong>strumental to enhanc<strong>in</strong>g susta<strong>in</strong>ability, efficiency and most notably <strong>equity</strong>.<br />
We therefore do not mention it separately (see also Bijlmakers, 2003).<br />
8 The reviewed literature mentions different strategies for such quality improvement: either directly or <strong>in</strong>directly<br />
aimed at <strong>health</strong> services. Kipp et al (2001) report on the implementation <strong>of</strong> <strong>user</strong> <strong>fees</strong> as a staff <strong>in</strong>centive system<br />
(i.e. top up low salaries), which led <strong>health</strong> workers to <strong>of</strong>fer improved services. They note that they found no other<br />
published <strong>in</strong>formation on us<strong>in</strong>g cost-shar<strong>in</strong>g revenues <strong>in</strong> such a way.<br />
Equity Implications <strong>of</strong> Health Sector User Fees <strong>in</strong> Tanzania 3