equity implications of health sector user fees in tanzania
equity implications of health sector user fees in tanzania
equity implications of health sector user fees in tanzania
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
and Health <strong>in</strong> Sub-Sahara Africa (Addis Ababa 20 June 1997) has been <strong>in</strong>cluded <strong>in</strong> the Technical<br />
Paper Part 4. The follow<strong>in</strong>g overview <strong>of</strong> key f<strong>in</strong>d<strong>in</strong>gs follows Gilson (1997; cit<strong>in</strong>g various authors) 9 and<br />
has been supplemented with observations from the literature review.<br />
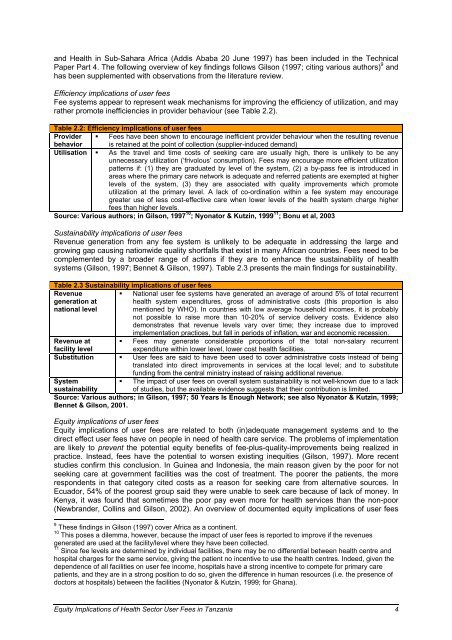
Efficiency <strong>implications</strong> <strong>of</strong> <strong>user</strong> <strong>fees</strong><br />
Fee systems appear to represent weak mechanisms for improv<strong>in</strong>g the efficiency <strong>of</strong> utilization, and may<br />
rather promote <strong>in</strong>efficiencies <strong>in</strong> provider behaviour (see Table 2.2).<br />
Table 2.2: Efficiency <strong>implications</strong> <strong>of</strong> <strong>user</strong> <strong>fees</strong><br />
Provider � Fees have been shown to encourage <strong>in</strong>efficient provider behaviour when the result<strong>in</strong>g revenue<br />
behavior is reta<strong>in</strong>ed at the po<strong>in</strong>t <strong>of</strong> collection (supplier-<strong>in</strong>duced demand)<br />
Utilisation � As the travel and time costs <strong>of</strong> seek<strong>in</strong>g care are usually high, there is unlikely to be any<br />
unnecessary utilization (‘frivolous’ consumption). Fees may encourage more efficient utilization<br />
patterns if: (1) they are graduated by level <strong>of</strong> the system, (2) a by-pass fee is <strong>in</strong>troduced <strong>in</strong><br />
areas where the primary care network is adequate and referred patients are exempted at higher<br />
levels <strong>of</strong> the system, (3) they are associated with quality improvements which promote<br />
utilization at the primary level. A lack <strong>of</strong> co-ord<strong>in</strong>ation with<strong>in</strong> a fee system may encourage<br />
greater use <strong>of</strong> less cost-effective care when lower levels <strong>of</strong> the <strong>health</strong> system charge higher<br />
<strong>fees</strong> than higher levels.<br />
Source: Various authors; <strong>in</strong> Gilson, 1997 10 ; Nyonator & Kutz<strong>in</strong>, 1999 11 ; Bonu et al, 2003<br />
Susta<strong>in</strong>ability <strong>implications</strong> <strong>of</strong> <strong>user</strong> <strong>fees</strong><br />
Revenue generation from any fee system is unlikely to be adequate <strong>in</strong> address<strong>in</strong>g the large and<br />
grow<strong>in</strong>g gap caus<strong>in</strong>g nationwide quality shortfalls that exist <strong>in</strong> many African countries. Fees need to be<br />
complemented by a broader range <strong>of</strong> actions if they are to enhance the susta<strong>in</strong>ability <strong>of</strong> <strong>health</strong><br />
systems (Gilson, 1997; Bennet & Gilson, 1997). Table 2.3 presents the ma<strong>in</strong> f<strong>in</strong>d<strong>in</strong>gs for susta<strong>in</strong>ability.<br />
Table 2.3 Susta<strong>in</strong>ability <strong>implications</strong> <strong>of</strong> <strong>user</strong> <strong>fees</strong><br />
Revenue<br />
generation at<br />
national level<br />
� National <strong>user</strong> fee systems have generated an average <strong>of</strong> around 5% <strong>of</strong> total recurrent<br />
<strong>health</strong> system expenditures, gross <strong>of</strong> adm<strong>in</strong>istrative costs (this proportion is also<br />
mentioned by WHO). In countries with low average household <strong>in</strong>comes, it is probably<br />
not possible to raise more than 10-20% <strong>of</strong> service delivery costs. Evidence also<br />
demonstrates that revenue levels vary over time; they <strong>in</strong>crease due to improved<br />
implementation practices, but fall <strong>in</strong> periods <strong>of</strong> <strong>in</strong>flation, war and economic recession.<br />
Revenue at � Fees may generate considerable proportions <strong>of</strong> the total non-salary recurrent<br />
facility level<br />
expenditure with<strong>in</strong> lower level, lower cost <strong>health</strong> facilities.<br />
Substitution � User <strong>fees</strong> are said to have been used to cover adm<strong>in</strong>istrative costs <strong>in</strong>stead <strong>of</strong> be<strong>in</strong>g<br />
translated <strong>in</strong>to direct improvements <strong>in</strong> services at the local level; and to substitute<br />
fund<strong>in</strong>g from the central m<strong>in</strong>istry <strong>in</strong>stead <strong>of</strong> rais<strong>in</strong>g additional revenue.<br />
System<br />
� The impact <strong>of</strong> <strong>user</strong> <strong>fees</strong> on overall system susta<strong>in</strong>ability is not well-known due to a lack<br />
susta<strong>in</strong>ability<br />
<strong>of</strong> studies, but the available evidence suggests that their contribution is limited.<br />
Source: Various authors; <strong>in</strong> Gilson, 1997; 50 Years Is Enough Network; see also Nyonator & Kutz<strong>in</strong>, 1999;<br />
Bennet & Gilson, 2001.<br />
Equity <strong>implications</strong> <strong>of</strong> <strong>user</strong> <strong>fees</strong><br />
Equity <strong>implications</strong> <strong>of</strong> <strong>user</strong> <strong>fees</strong> are related to both (<strong>in</strong>)adequate management systems and to the<br />
direct effect <strong>user</strong> <strong>fees</strong> have on people <strong>in</strong> need <strong>of</strong> <strong>health</strong> care service. The problems <strong>of</strong> implementation<br />
are likely to prevent the potential <strong>equity</strong> benefits <strong>of</strong> fee-plus-quality-improvements be<strong>in</strong>g realized <strong>in</strong><br />
practice. Instead, <strong>fees</strong> have the potential to worsen exist<strong>in</strong>g <strong>in</strong>equities (Gilson, 1997). More recent<br />
studies confirm this conclusion. In Gu<strong>in</strong>ea and Indonesia, the ma<strong>in</strong> reason given by the poor for not<br />
seek<strong>in</strong>g care at government facilities was the cost <strong>of</strong> treatment. The poorer the patients, the more<br />
respondents <strong>in</strong> that category cited costs as a reason for seek<strong>in</strong>g care from alternative sources. In<br />
Ecuador, 54% <strong>of</strong> the poorest group said they were unable to seek care because <strong>of</strong> lack <strong>of</strong> money. In<br />
Kenya, it was found that sometimes the poor pay even more for <strong>health</strong> services than the non-poor<br />
(Newbrander, Coll<strong>in</strong>s and Gilson, 2002). An overview <strong>of</strong> documented <strong>equity</strong> <strong>implications</strong> <strong>of</strong> <strong>user</strong> <strong>fees</strong><br />
9 These f<strong>in</strong>d<strong>in</strong>gs <strong>in</strong> Gilson (1997) cover Africa as a cont<strong>in</strong>ent.<br />
10 This poses a dilemma, however, because the impact <strong>of</strong> <strong>user</strong> <strong>fees</strong> is reported to improve if the revenues<br />
generated are used at the facility/level where they have been collected.<br />
11 S<strong>in</strong>ce fee levels are determ<strong>in</strong>ed by <strong>in</strong>dividual facilities, there may be no differential between <strong>health</strong> centre and<br />
hospital charges for the same service, giv<strong>in</strong>g the patient no <strong>in</strong>centive to use the <strong>health</strong> centres. Indeed, given the<br />
dependence <strong>of</strong> all facilities on <strong>user</strong> fee <strong>in</strong>come, hospitals have a strong <strong>in</strong>centive to compete for primary care<br />
patients, and they are <strong>in</strong> a strong position to do so, given the difference <strong>in</strong> human resources (i.e. the presence <strong>of</strong><br />
doctors at hospitals) between the facilities (Nyonator & Kutz<strong>in</strong>, 1999; for Ghana).<br />
Equity Implications <strong>of</strong> Health Sector User Fees <strong>in</strong> Tanzania 4