equity implications of health sector user fees in tanzania
equity implications of health sector user fees in tanzania
equity implications of health sector user fees in tanzania
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Pro-poor observations<br />
Tanzania has undertaken important measures to strengthen its pro-poor f<strong>in</strong>anc<strong>in</strong>g strategies <strong>in</strong> the<br />
<strong>health</strong> <strong>sector</strong>. Various documents reflect exist<strong>in</strong>g pro-poor expenditure mechanisms (REPOA 2001,<br />
MOH/SDC2001, MOH/DFID 2002, Poverty and Human Development Report, PER 2004; see table<br />
4.3). Resource allocations may be considered to be pro-poor if they put priority on address<strong>in</strong>g the<br />
burden <strong>of</strong> diseases which disproportionately affect poor people 25 and an <strong>in</strong>creased provision <strong>of</strong><br />
essential medical supplies and drugs (the latter is covered <strong>in</strong> the budget under the head<strong>in</strong>g Other<br />
Charges (OC)) (Poverty Human Development Report 2002:80). The new Equitable Resource<br />
Allocation Formula (ERAF) takes the pro-poor allocations <strong>in</strong>to consideration as well. The ERAF aims<br />
to redirect resources towards the poor, the rural areas and priorities <strong>of</strong> the <strong>health</strong> <strong>sector</strong>. This is a clear<br />
pro-poor approach which is <strong>in</strong> l<strong>in</strong>e with PRS objectives and the National Health Policy 2002.<br />
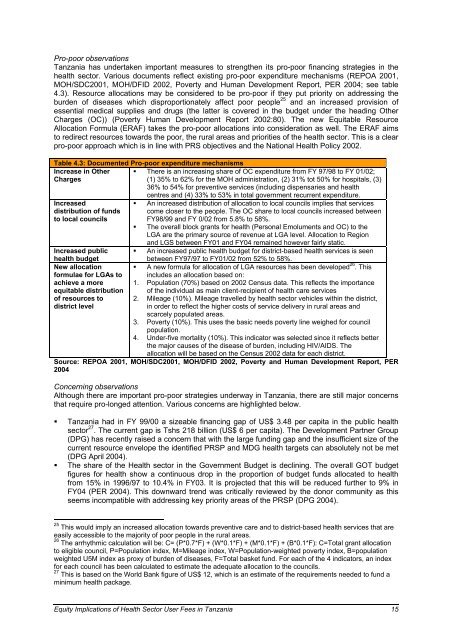
Table 4.3: Documented Pro-poor expenditure mechanisms<br />
Increase <strong>in</strong> Other<br />
Charges<br />
Increased<br />
distribution <strong>of</strong> funds<br />
to local councils<br />
� There is an <strong>in</strong>creas<strong>in</strong>g share <strong>of</strong> OC expenditure from FY 97/98 to FY 01/02;<br />
(1) 35% to 62% for the MOH adm<strong>in</strong>istration, (2) 31% tot 50% for hospitals, (3)<br />
36% to 54% for preventive services (<strong>in</strong>clud<strong>in</strong>g dispensaries and <strong>health</strong><br />
centres and (4) 33% to 53% <strong>in</strong> total government recurrent expenditure.<br />
� An <strong>in</strong>creased distribution <strong>of</strong> allocation to local councils implies that services<br />
come closer to the people. The OC share to local councils <strong>in</strong>creased between<br />
FY98/99 and FY 0/02 from 5.8% to 58%.<br />
� The overall block grants for <strong>health</strong> (Personal Emoluments and OC) to the<br />
LGA are the primary source <strong>of</strong> revenue at LGA level. Allocation to Region<br />
and LGS between FY01 and FY04 rema<strong>in</strong>ed however fairly static.<br />
� An <strong>in</strong>creased public <strong>health</strong> budget for district-based <strong>health</strong> services is seen<br />
Increased public<br />
<strong>health</strong> budget<br />
between FY97/97 to FY01/02 from 52% to 58%.<br />
New allocation � A new formula for allocation <strong>of</strong> LGA resources has been developed<br />
formulae for LGAs to<br />
achieve a more<br />
equitable distribution<br />
<strong>of</strong> resources to<br />
district level<br />
26 . This<br />
<strong>in</strong>cludes an allocation based on:<br />
1. Population (70%) based on 2002 Census data. This reflects the importance<br />
<strong>of</strong> the <strong>in</strong>dividual as ma<strong>in</strong> client-recipient <strong>of</strong> <strong>health</strong> care services<br />
2. Mileage (10%). Mileage travelled by <strong>health</strong> <strong>sector</strong> vehicles with<strong>in</strong> the district,<br />
<strong>in</strong> order to reflect the higher costs <strong>of</strong> service delivery <strong>in</strong> rural areas and<br />
scarcely populated areas.<br />
3. Poverty (10%). This uses the basic needs poverty l<strong>in</strong>e weighed for council<br />
population.<br />
4. Under-five mortality (10%). This <strong>in</strong>dicator was selected s<strong>in</strong>ce it reflects better<br />
the major causes <strong>of</strong> the disease <strong>of</strong> burden, <strong>in</strong>clud<strong>in</strong>g HIV/AIDS. The<br />
allocation will be based on the Census 2002 data for each district.<br />
Source: REPOA 2001, MOH/SDC2001, MOH/DFID 2002, Poverty and Human Development Report, PER<br />
2004<br />
Concern<strong>in</strong>g observations<br />
Although there are important pro-poor strategies underway <strong>in</strong> Tanzania, there are still major concerns<br />
that require pro-longed attention. Various concerns are highlighted below.<br />
� Tanzania had <strong>in</strong> FY 99/00 a sizeable f<strong>in</strong>anc<strong>in</strong>g gap <strong>of</strong> US$ 3.48 per capita <strong>in</strong> the public <strong>health</strong><br />
<strong>sector</strong> 27 . The current gap is Tshs 218 billion (US$ 6 per capita). The Development Partner Group<br />
(DPG) has recently raised a concern that with the large fund<strong>in</strong>g gap and the <strong>in</strong>sufficient size <strong>of</strong> the<br />
current resource envelope the identified PRSP and MDG <strong>health</strong> targets can absolutely not be met<br />
(DPG April 2004).<br />
� The share <strong>of</strong> the Health <strong>sector</strong> <strong>in</strong> the Government Budget is decl<strong>in</strong><strong>in</strong>g. The overall GOT budget<br />
figures for <strong>health</strong> show a cont<strong>in</strong>uous drop <strong>in</strong> the proportion <strong>of</strong> budget funds allocated to <strong>health</strong><br />
from 15% <strong>in</strong> 1996/97 to 10.4% <strong>in</strong> FY03. It is projected that this will be reduced further to 9% <strong>in</strong><br />
FY04 (PER 2004). This downward trend was critically reviewed by the donor community as this<br />
seems <strong>in</strong>compatible with address<strong>in</strong>g key priority areas <strong>of</strong> the PRSP (DPG 2004).<br />
25<br />
This would imply an <strong>in</strong>creased allocation towards preventive care and to district-based <strong>health</strong> services that are<br />
easily accessible to the majority <strong>of</strong> poor people <strong>in</strong> the rural areas.<br />
26<br />
The arrhythmic calculation will be: C= (P*0.7*F) + (W*0.1*F) + (M*0.1*F) + (B*0.1*F): C=Total grant allocation<br />
to eligible council, P=Population <strong>in</strong>dex, M=Mileage <strong>in</strong>dex, W=Population-weighted poverty <strong>in</strong>dex, B=population<br />
weighted U5M <strong>in</strong>dex as proxy <strong>of</strong> burden <strong>of</strong> diseases, F=Total basket fund. For each <strong>of</strong> the 4 <strong>in</strong>dicators, an <strong>in</strong>dex<br />
for each council has been calculated to estimate the adequate allocation to the councils.<br />
27<br />
This is based on the World Bank figure <strong>of</strong> US$ 12, which is an estimate <strong>of</strong> the requirements needed to fund a<br />
m<strong>in</strong>imum <strong>health</strong> package.<br />
Equity Implications <strong>of</strong> Health Sector User Fees <strong>in</strong> Tanzania 15