equity implications of health sector user fees in tanzania
equity implications of health sector user fees in tanzania
equity implications of health sector user fees in tanzania
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Critical factors that hamper access to <strong>health</strong> services<br />
The study <strong>of</strong> Mubyazi et al (2002) reflected <strong>in</strong>come levels <strong>in</strong> Kagera. These could be divided <strong>in</strong>to (1)<br />
people with a monthly <strong>in</strong>come <strong>of</strong> less than Tshs. 5,000/= (29%), (2) people with a monthly <strong>in</strong>come<br />
between Tshs. 5,000/= - 10,000/= (30%) and (3) people with a monthly <strong>in</strong>come <strong>of</strong> less than Tshs.<br />
16,000/= (69%) <strong>of</strong> the respondents. People with an <strong>in</strong>come <strong>of</strong> Tshs. 5,000 or less live ma<strong>in</strong>ly <strong>in</strong> the<br />
rural areas. Critical factors that prevented people from adequate access and use <strong>of</strong> <strong>health</strong> facilities<br />
<strong>in</strong>cluded (1) liv<strong>in</strong>g <strong>in</strong> a rural area (only 19% report access with<strong>in</strong> 30 m<strong>in</strong>utes walk<strong>in</strong>g), (2) distance as a<br />
deterrent to use <strong>health</strong> services (15% <strong>in</strong> rural areas), (3) costs <strong>of</strong> transport for people liv<strong>in</strong>g far from a<br />
<strong>health</strong> facility (31%), (4) costs <strong>of</strong> treatment as a deterrent to use (47-60% <strong>of</strong> the population not seek<strong>in</strong>g<br />
<strong>health</strong> care while ill), (5) deteriorated quality <strong>of</strong> services especially at peripheral <strong>health</strong> facilities<br />
(availability <strong>of</strong> drugs, shortage <strong>of</strong> staff), (6) age (23% <strong>of</strong> the people older then 60 years live with<strong>in</strong> 30<br />
m<strong>in</strong>utes <strong>of</strong> a <strong>health</strong> facility and (7) gender-poverty status. Women from poor households a remote<br />
likely to give birth at home than women from non-poor households (Mubyazi et al, 2002 and CWIQ<br />
survey, 2004).<br />
6.5 F<strong>in</strong>d<strong>in</strong>gs from the assessment carried out by the study team, 2004<br />
Exclusion <strong>of</strong> vulnerable groups and poor people<br />
The study team collected addition data <strong>in</strong> March 2004. Interviews with poor people and specific<br />
categories <strong>of</strong> vulnerable people revealed that people are excluded from access to <strong>health</strong> services. The<br />
<strong>equity</strong> <strong>implications</strong> <strong>of</strong> <strong>user</strong> <strong>fees</strong> show that the poorest people cannot afford to pay the <strong>user</strong> <strong>fees</strong>. The<br />
poorest people <strong>in</strong>dicated that they could not afford the payment <strong>of</strong> Tshs. 400/= for a card <strong>in</strong> a public<br />
<strong>health</strong> facility. For this, people depend on support <strong>of</strong> their relatives, the sale <strong>of</strong> private property or the<br />
support from an NGO supported programme. The groups which systematically face exclusion <strong>of</strong> basic<br />
<strong>health</strong> services are; (1) Orphans, (2) Widows, (3) AIDS clients, (4) Elderly, (5) People with disabilities,<br />
(6) Pregnant women and (7) under-five children. Equal access to <strong>health</strong> services is prevented by; (1)<br />
poverty, (2) geographical barriers and distance, (3) gender aspects, (4) demotivated <strong>health</strong> staff and<br />
(5) <strong>in</strong>formal charges. It was reported that unequal access has contributed to; (1) delayed and<br />
<strong>in</strong>adequate treatment, (2) sale <strong>of</strong> private property, (3) reduced food <strong>in</strong>take (to save money), (4) child<br />
labour and (5) petty crime (to generate money). The poorest people <strong>in</strong>dicate they have better access<br />
to the public HFs because <strong>of</strong> the lower <strong>user</strong> fee level. It is felt that there is a higher chance to get a<br />
waiver <strong>in</strong> a public HF. Table 6.4 and 6.5 provide experiences <strong>of</strong> 10 HIV positive clients and 8 disabled<br />
people.<br />
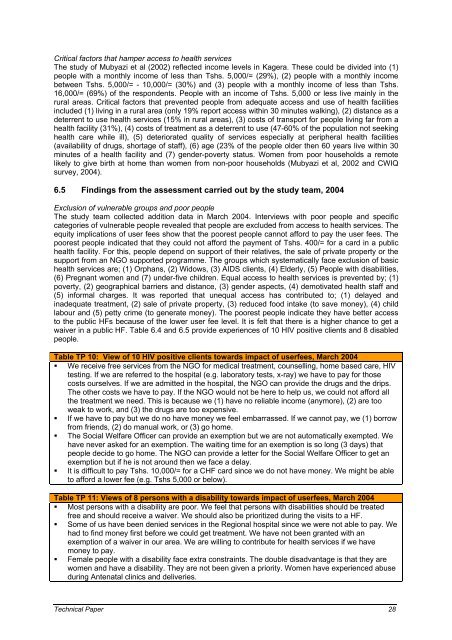
Table TP 10: View <strong>of</strong> 10 HIV positive clients towards impact <strong>of</strong> <strong>user</strong><strong>fees</strong>, March 2004<br />
� We receive free services from the NGO for medical treatment, counsell<strong>in</strong>g, home based care, HIV<br />
test<strong>in</strong>g. If we are referred to the hospital (e.g. laboratory tests, x-ray) we have to pay for those<br />
costs ourselves. If we are admitted <strong>in</strong> the hospital, the NGO can provide the drugs and the drips.<br />
The other costs we have to pay. If the NGO would not be here to help us, we could not afford all<br />
the treatment we need. This is because we (1) have no reliable <strong>in</strong>come (anymore), (2) are too<br />
weak to work, and (3) the drugs are too expensive.<br />
� If we have to pay but we do no have money we feel embarrassed. If we cannot pay, we (1) borrow<br />
from friends, (2) do manual work, or (3) go home.<br />
� The Social Welfare Officer can provide an exemption but we are not automatically exempted. We<br />
have never asked for an exemption. The wait<strong>in</strong>g time for an exemption is so long (3 days) that<br />
people decide to go home. The NGO can provide a letter for the Social Welfare Officer to get an<br />
exemption but if he is not around then we face a delay.<br />
� It is difficult to pay Tshs. 10,000/= for a CHF card s<strong>in</strong>ce we do not have money. We might be able<br />
to afford a lower fee (e.g. Tshs 5,000 or below).<br />
Table TP 11: Views <strong>of</strong> 8 persons with a disability towards impact <strong>of</strong> <strong>user</strong><strong>fees</strong>, March 2004<br />
� Most persons with a disability are poor. We feel that persons with disabilities should be treated<br />
free and should receive a waiver. We should also be prioritized dur<strong>in</strong>g the visits to a HF.<br />
� Some <strong>of</strong> us have been denied services <strong>in</strong> the Regional hospital s<strong>in</strong>ce we were not able to pay. We<br />
had to f<strong>in</strong>d money first before we could get treatment. We have not been granted with an<br />
exemption <strong>of</strong> a waiver <strong>in</strong> our area. We are will<strong>in</strong>g to contribute for <strong>health</strong> services if we have<br />
money to pay.<br />
� Female people with a disability face extra constra<strong>in</strong>ts. The double disadvantage is that they are<br />
women and have a disability. They are not been given a priority. Women have experienced abuse<br />
dur<strong>in</strong>g Antenatal cl<strong>in</strong>ics and deliveries.<br />
Technical Paper 28