MERCOLEDI' 5 OTTOBRE SALA C ORE 9 - Avenue media
MERCOLEDI' 5 OTTOBRE SALA C ORE 9 - Avenue media
MERCOLEDI' 5 OTTOBRE SALA C ORE 9 - Avenue media
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
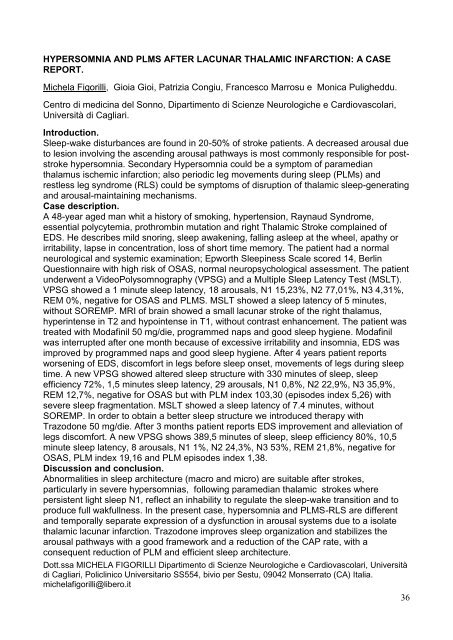
HYPERSOMNIA AND PLMS AFTER LACUNAR THALAMIC INFARCTION: A CASE<br />
REPORT.<br />
Michela Figorilli, Gioia Gioi, Patrizia Congiu, Francesco Marrosu e Monica Puligheddu.<br />
Centro di medicina del Sonno, Dipartimento di Scienze Neurologiche e Cardiovascolari,<br />
Università di Cagliari.<br />
Introduction.<br />
Sleep-wake disturbances are found in 20-50% of stroke patients. A decreased arousal due<br />
to lesion involving the ascending arousal pathways is most commonly responsible for poststroke<br />
hypersomnia. Secondary Hypersomnia could be a symptom of para<strong>media</strong>n<br />
thalamus ischemic infarction; also periodic leg movements during sleep (PLMs) and<br />
restless leg syndrome (RLS) could be symptoms of disruption of thalamic sleep-generating<br />
and arousal-maintaining mechanisms.<br />
Case description.<br />
A 48-year aged man whit a history of smoking, hypertension, Raynaud Syndrome,<br />
essential polycytemia, prothrombin mutation and right Thalamic Stroke complained of<br />
EDS. He describes mild snoring, sleep awakening, falling asleep at the wheel, apathy or<br />
irritability, lapse in concentration, loss of short time memory. The patient had a normal<br />
neurological and systemic examination; Epworth Sleepiness Scale scored 14, Berlin<br />
Questionnaire with high risk of OSAS, normal neuropsychological assessment. The patient<br />
underwent a VideoPolysomnography (VPSG) and a Multiple Sleep Latency Test (MSLT).<br />
VPSG showed a 1 minute sleep latency, 18 arousals, N1 15,23%, N2 77,01%, N3 4,31%,<br />
REM 0%, negative for OSAS and PLMS. MSLT showed a sleep latency of 5 minutes,<br />
without S<strong>ORE</strong>MP. MRI of brain showed a small lacunar stroke of the right thalamus,<br />
hyperintense in T2 and hypointense in T1, without contrast enhancement. The patient was<br />
treated with Modafinil 50 mg/die, programmed naps and good sleep hygiene. Modafinil<br />
was interrupted after one month because of excessive irritability and insomnia, EDS was<br />
improved by programmed naps and good sleep hygiene. After 4 years patient reports<br />
worsening of EDS, discomfort in legs before sleep onset, movements of legs during sleep<br />
time. A new VPSG showed altered sleep structure with 330 minutes of sleep, sleep<br />
efficiency 72%, 1,5 minutes sleep latency, 29 arousals, N1 0,8%, N2 22,9%, N3 35,9%,<br />
REM 12,7%, negative for OSAS but with PLM index 103,30 (episodes index 5,26) with<br />
severe sleep fragmentation. MSLT showed a sleep latency of 7.4 minutes, without<br />
S<strong>ORE</strong>MP. In order to obtain a better sleep structure we introduced therapy with<br />
Trazodone 50 mg/die. After 3 months patient reports EDS improvement and alleviation of<br />
legs discomfort. A new VPSG shows 389,5 minutes of sleep, sleep efficiency 80%, 10,5<br />
minute sleep latency, 8 arousals, N1 1%, N2 24,3%, N3 53%, REM 21,8%, negative for<br />
OSAS, PLM index 19,16 and PLM episodes index 1,38.<br />
Discussion and conclusion.<br />
Abnormalities in sleep architecture (macro and micro) are suitable after strokes,<br />
particularly in severe hypersomnias, following para<strong>media</strong>n thalamic strokes where<br />
persistent light sleep N1, reflect an inhability to regulate the sleep-wake transition and to<br />
produce full wakfullness. In the present case, hypersomnia and PLMS-RLS are different<br />
and temporally separate expression of a dysfunction in arousal systems due to a isolate<br />
thalamic lacunar infarction. Trazodone improves sleep organization and stabilizes the<br />
arousal pathways with a good framework and a reduction of the CAP rate, with a<br />
consequent reduction of PLM and efficient sleep architecture.<br />
Dott.ssa MICHELA FIGORILLI Dipartimento di Scienze Neurologiche e Cardiovascolari, Università<br />
di Cagliari, Policlinico Universitario SS554, bivio per Sestu, 09042 Monserrato (CA) Italia.<br />
michelafigorilli@libero.it<br />
36