Insomnia Insomnia
Insomnia Insomnia
Insomnia Insomnia
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Insomnia</strong> in Psychiatric Disorders 129<br />
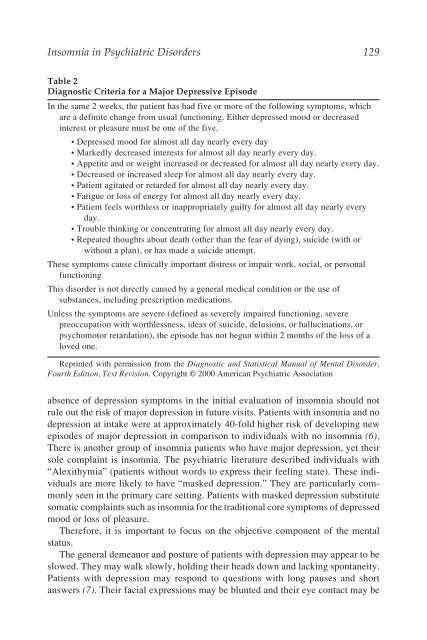
Table 2<br />
Diagnostic Criteria for a Major Depressive Episode<br />
In the same 2 weeks, the patient has had five or more of the following symptoms, which<br />
are a definite change from usual functioning. Either depressed mood or decreased<br />
interest or pleasure must be one of the five.<br />
• Depressed mood for almost all day nearly every day<br />
• Markedly decreased interests for almost all day nearly every day.<br />
• Appetite and or weight increased or decreased for almost all day nearly every day.<br />
• Decreased or increased sleep for almost all day nearly every day.<br />
• Patient agitated or retarded for almost all day nearly every day.<br />
• Fatigue or loss of energy for almost all day nearly every day.<br />
• Patient feels worthless or inappropriately guilty for almost all day nearly every<br />
day.<br />
• Trouble thinking or concentrating for almost all day nearly every day.<br />
• Repeated thoughts about death (other than the fear of dying), suicide (with or<br />
without a plan), or has made a suicide attempt.<br />
These symptoms cause clinically important distress or impair work, social, or personal<br />
functioning<br />
This disorder is not directly caused by a general medical condition or the use of<br />
substances, including prescription medications.<br />
Unless the symptoms are severe (defined as severely impaired functioning, severe<br />
preoccupation with worthlessness, ideas of suicide, delusions, or hallucinations, or<br />
psychomotor retardation), the episode has not begun within 2 months of the loss of a<br />
loved one.<br />
Reprinted with permission from the Diagnostic and Statistical Manual of Mental Disorder,<br />
Fourth Edition, Text Revision. Copyright © 2000 American Psychiatric Association<br />
absence of depression symptoms in the initial evaluation of insomnia should not<br />
rule out the risk of major depression in future visits. Patients with insomnia and no<br />
depression at intake were at approximately 40-fold higher risk of developing new<br />
episodes of major depression in comparison to individuals with no insomnia (6).<br />
There is another group of insomnia patients who have major depression, yet their<br />
sole complaint is insomnia. The psychiatric literature described individuals with<br />
“Alexithymia” (patients without words to express their feeling state). These individuals<br />
are more likely to have “masked depression.” They are particularly commonly<br />
seen in the primary care setting. Patients with masked depression substitute<br />
somatic complaints such as insomnia for the traditional core symptoms of depressed<br />
mood or loss of pleasure.<br />
Therefore, it is important to focus on the objective component of the mental<br />
status.<br />
The general demeanor and posture of patients with depression may appear to be<br />
slowed. They may walk slowly, holding their heads down and lacking spontaneity.<br />
Patients with depression may respond to questions with long pauses and short<br />
answers (7). Their facial expressions may be blunted and their eye contact may be