Insomnia Insomnia
Insomnia Insomnia
Insomnia Insomnia
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
24 Bonnet and Arand<br />
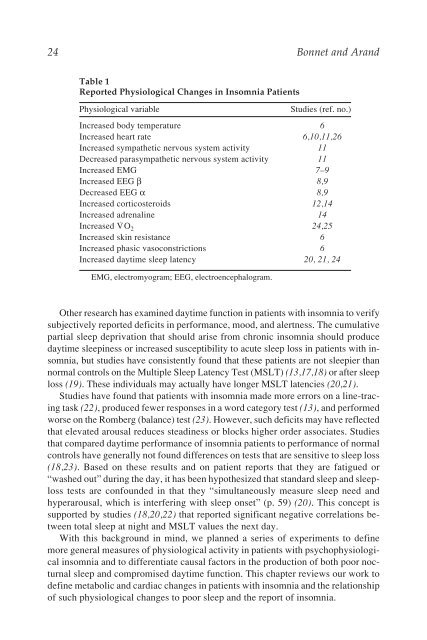
Table 1<br />
Reported Physiological Changes in <strong>Insomnia</strong> Patients<br />
Physiological variable Studies (ref. no.)<br />
Increased body temperature 6<br />
Increased heart rate 6,10,11,26<br />
Increased sympathetic nervous system activity 11<br />
Decreased parasympathetic nervous system activity 11<br />
Increased EMG 7–9<br />
Increased EEG β 8,9<br />
Decreased EEG α 8,9<br />
Increased corticosteroids 12,14<br />
Increased adrenaline<br />
Increased V<br />
14<br />
·<br />
O2 24,25<br />
Increased skin resistance 6<br />
Increased phasic vasoconstrictions 6<br />
Increased daytime sleep latency 20, 21, 24<br />
EMG, electromyogram; EEG, electroencephalogram.<br />
Other research has examined daytime function in patients with insomnia to verify<br />
subjectively reported deficits in performance, mood, and alertness. The cumulative<br />
partial sleep deprivation that should arise from chronic insomnia should produce<br />
daytime sleepiness or increased susceptibility to acute sleep loss in patients with insomnia,<br />
but studies have consistently found that these patients are not sleepier than<br />
normal controls on the Multiple Sleep Latency Test (MSLT) (13,17,18) or after sleep<br />
loss (19). These individuals may actually have longer MSLT latencies (20,21).<br />
Studies have found that patients with insomnia made more errors on a line-tracing<br />
task (22), produced fewer responses in a word category test (13), and performed<br />
worse on the Romberg (balance) test (23). However, such deficits may have reflected<br />
that elevated arousal reduces steadiness or blocks higher order associates. Studies<br />
that compared daytime performance of insomnia patients to performance of normal<br />
controls have generally not found differences on tests that are sensitive to sleep loss<br />
(18,23). Based on these results and on patient reports that they are fatigued or<br />
“washed out” during the day, it has been hypothesized that standard sleep and sleeploss<br />
tests are confounded in that they “simultaneously measure sleep need and<br />
hyperarousal, which is interfering with sleep onset” (p. 59) (20). This concept is<br />
supported by studies (18,20,22) that reported significant negative correlations between<br />
total sleep at night and MSLT values the next day.<br />
With this background in mind, we planned a series of experiments to define<br />
more general measures of physiological activity in patients with psychophysiological<br />
insomnia and to differentiate causal factors in the production of both poor nocturnal<br />
sleep and compromised daytime function. This chapter reviews our work to<br />
define metabolic and cardiac changes in patients with insomnia and the relationship<br />
of such physiological changes to poor sleep and the report of insomnia.