Het volume van chirurgische ingrepen en de impact ervan op ... - KCE
Het volume van chirurgische ingrepen en de impact ervan op ... - KCE
Het volume van chirurgische ingrepen en de impact ervan op ... - KCE
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>KCE</strong> Reports 113 Volume Outcome 167<br />
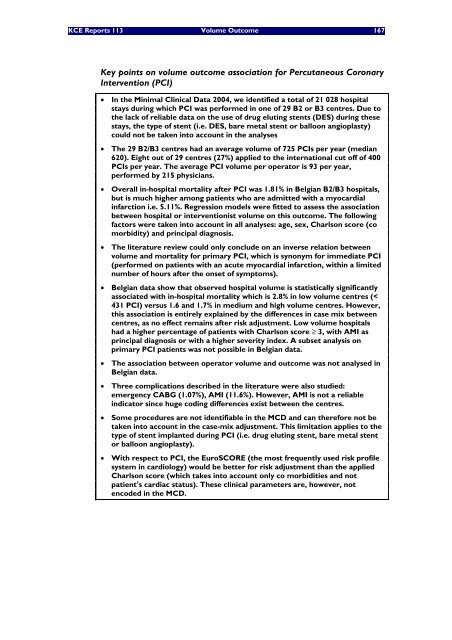
Key points on <strong>volume</strong> outcome association for Percutaneous Coronary<br />
Interv<strong>en</strong>tion (PCI)<br />
• In the Minimal Clinical Data 2004, we id<strong>en</strong>tified a total of 21 028 hospital<br />
stays during which PCI was performed in one of 29 B2 or B3 c<strong>en</strong>tres. Due to<br />
the lack of reliable data on the use of drug eluting st<strong>en</strong>ts (DES) during these<br />
stays, the type of st<strong>en</strong>t (i.e. DES, bare metal st<strong>en</strong>t or balloon angi<strong>op</strong>lasty)<br />
could not be tak<strong>en</strong> into account in the analyses<br />
• The 29 B2/B3 c<strong>en</strong>tres had an average <strong>volume</strong> of 725 PCIs per year (median<br />
620). Eight out of 29 c<strong>en</strong>tres (27%) applied to the international cut off of 400<br />
PCIs per year. The average PCI <strong>volume</strong> per <strong>op</strong>erator is 93 per year,<br />
performed by 215 physicians.<br />
• Overall in-hospital mortality after PCI was 1.81% in Belgian B2/B3 hospitals,<br />
but is much higher among pati<strong>en</strong>ts who are admitted with a myocardial<br />
infarction i.e. 5.11%. Regression mo<strong>de</strong>ls were fitted to assess the association<br />
betwe<strong>en</strong> hospital or interv<strong>en</strong>tionist <strong>volume</strong> on this outcome. The following<br />
factors were tak<strong>en</strong> into account in all analyses: age, sex, Charlson score (co<br />
morbidity) and principal diagnosis.<br />
• The literature review could only conclu<strong>de</strong> on an inverse relation betwe<strong>en</strong><br />
<strong>volume</strong> and mortality for primary PCI, which is synonym for immediate PCI<br />
(performed on pati<strong>en</strong>ts with an acute myocardial infarction, within a limited<br />
number of hours after the onset of symptoms).<br />
• Belgian data show that observed hospital <strong>volume</strong> is statistically significantly<br />
associated with in-hospital mortality which is 2.8% in low <strong>volume</strong> c<strong>en</strong>tres (<<br />
431 PCI) versus 1.6 and 1.7% in medium and high <strong>volume</strong> c<strong>en</strong>tres. However,<br />
this association is <strong>en</strong>tirely explained by the differ<strong>en</strong>ces in case mix betwe<strong>en</strong><br />
c<strong>en</strong>tres, as no effect remains after risk adjustm<strong>en</strong>t. Low <strong>volume</strong> hospitals<br />
had a higher perc<strong>en</strong>tage of pati<strong>en</strong>ts with Charlson score ≥ 3, with AMI as<br />
principal diagnosis or with a higher severity in<strong>de</strong>x. A subset analysis on<br />
primary PCI pati<strong>en</strong>ts was not possible in Belgian data.<br />
• The association betwe<strong>en</strong> <strong>op</strong>erator <strong>volume</strong> and outcome was not analysed in<br />
Belgian data.<br />
• Three complications <strong>de</strong>scribed in the literature were also studied:<br />
emerg<strong>en</strong>cy CABG (1.07%), AMI (11.6%). However, AMI is not a reliable<br />
indicator since huge coding differ<strong>en</strong>ces exist betwe<strong>en</strong> the c<strong>en</strong>tres.<br />
• Some procedures are not id<strong>en</strong>tifiable in the MCD and can therefore not be<br />
tak<strong>en</strong> into account in the case-mix adjustm<strong>en</strong>t. This limitation applies to the<br />
type of st<strong>en</strong>t implanted during PCI (i.e. drug eluting st<strong>en</strong>t, bare metal st<strong>en</strong>t<br />
or balloon angi<strong>op</strong>lasty).<br />
• With respect to PCI, the EuroSCORE (the most frequ<strong>en</strong>tly used risk profile<br />
system in cardiology) would be better for risk adjustm<strong>en</strong>t than the applied<br />
Charlson score (which takes into account only co morbidities and not<br />
pati<strong>en</strong>t’s cardiac status). These clinical parameters are, however, not<br />
<strong>en</strong>co<strong>de</strong>d in the MCD.