Primary Retinal Detachment
Primary Retinal Detachment
Primary Retinal Detachment
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
84<br />
5 Vitrectomy for the <strong>Primary</strong> Management of <strong>Retinal</strong> <strong>Detachment</strong><br />
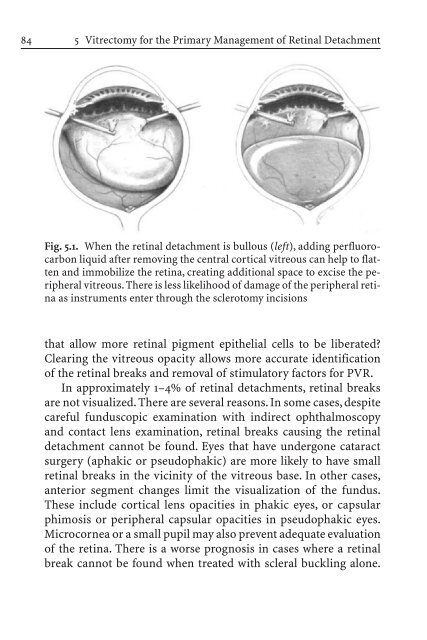
Fig. 5.1. When the retinal detachment is bullous (left), adding perfluorocarbon<br />
liquid after removing the central cortical vitreous can help to flatten<br />
and immobilize the retina, creating additional space to excise the peripheral<br />
vitreous. There is less likelihood of damage of the peripheral retina<br />
as instruments enter through the sclerotomy incisions<br />
that allow more retinal pigment epithelial cells to be liberated?<br />
Clearing the vitreous opacity allows more accurate identification<br />
of the retinal breaks and removal of stimulatory factors for PVR.<br />
In approximately 1–4% of retinal detachments, retinal breaks<br />
are not visualized. There are several reasons. In some cases, despite<br />
careful funduscopic examination with indirect ophthalmoscopy<br />
and contact lens examination, retinal breaks causing the retinal<br />
detachment cannot be found. Eyes that have undergone cataract<br />
surgery (aphakic or pseudophakic) are more likely to have small<br />
retinal breaks in the vicinity of the vitreous base. In other cases,<br />
anterior segment changes limit the visualization of the fundus.<br />
These include cortical lens opacities in phakic eyes, or capsular<br />
phimosis or peripheral capsular opacities in pseudophakic eyes.<br />
Microcornea or a small pupil may also prevent adequate evaluation<br />
of the retina. There is a worse prognosis in cases where a retinal<br />
break cannot be found when treated with scleral buckling alone.